The world of medicine seems like such a mystery no matter what side you're on. Sure, doctors see their fair share of common colds and broken bones, but every once in a while, a patient knocks them completely off their feet. These medical professionals came together to share the times that they've been stunned and stumped in the workplace—and they're both utterly bizarre and wildly interesting.
1. Caught In Her Throat
Primary doctor here. Had a two-year-old refugee child (whose parents couldn't communicate well) who swallowed a button battery and it was stuck in her throat. For clarity, I didn't know it was a button battery, but something just didn't feel right, so I sent her to the ED. If she had gone perhaps one more day, she might not have made it—it had already destroyed a good amount of tissue in her esophagus and was apparently somewhat close to perforating.
I feel like it would have been very easy to just say she had a sore throat from an illness, particularly with the language barrier. I'm glad that something felt weird to me—she didn't look that bad, but was just holding herself and breathing weirdly.
2. Ice Cold
A resident at my nursing home had hemorrhoids, and they were reportedly bleeding at the beginning of my shift. I called in some medicine for her, but it didn’t come in that night. When I checked on her, she seemed fine, so I assumed she could wait. I passed the information about the situation to the next shift and went home. That was a big mistake, apparently.
I got called into the office the next day and my boss yelled at me about it. I followed protocol and charted the situation accurately, so I was super confused about what the problem was. They then asked me, “Why didn't you just put an ice cube in her”?...WHAT. “An ice cube”? I exclaimed. “Yes,” they said, “Didn't you learn that in school”? Ummm no...
3. Infamous Last Words
I was a new nurse cleaning up a deceased patient. I went to turn her over and she let out a horrendous groan. Did know you could force air over the vocal cords of a cadaver? I did not, and I almost pooped myself in my scrubs.
4. Catching Zebras
My first rotation as a medical student was psychiatry. I was really nervous, and made a flashcard for each psych condition and a list of diagnoses to consider. One of the patients being discussed on rounds was psychotic (think: KGB is after me!) but was otherwise put together. He was really into doing art and was very, very religious.
I looked at my flashcard for psychosis and casually mentioned that we should consider temporal lobe epilepsy, which presents with religiosity and exaggerated artistic ability. An EEG showed that he had it. I've caught a few zebras since, but that was my favorite.
 Unsplash
Unsplash
5. Choose Your Words
We are taught to explain to patients exactly what we are doing, as we are doing it, so delicate wording becomes important during female pelvic exams. Instead of, "Okay, I am going to place the speculum inside now, so you'll just feel some warm pressure," my buddy—who was new at this—ended up saying "Okay, I'm going inside you now".
The female patient responds, "No thanks, I already have three children".
6. A Punch To The Gut
I used to be a pathology collector, so I basically collected patient bits and test them. One fellow needed some nail clippings and scrapings done for fungal testing. We used to see this a lot when it warmed up and people broke out their sandals...But this guy needed it for his hands. His nails were yellowed and starting to deform, and there was a smelly cheese-like substance under them.
Every. Single. Finger. It was the first and only time I ever had to try not to dry retch in front of a patient.
7. Unexpected Guests
Ordered an abdominal ultrasound on a refugee from Iraq via Syria, expecting to find gallstones because she felt full easily after eating and was having pain in her right upper quadrant. Instead of gallstones, there were two, 7 cm cysts in her liver. Hydatid cysts from a tapeworm.
8. Eye See What You Mean
I’m a doctor—an ophthalmologist to be exact. Recently, a young guy came to my office. He said he went to urgent care four times in 16 months or so for "pink eye". They convinced him it was just a coincidence that he got it four times. Well, the guy had blepharitis. Very common. Cracks me up.
9. At My Wit’s End
When I was a kid, another child in my class was institutionalized for acting out. After performing a routine workup and conducting some tests, I couldn't find anything wrong with him. According to the data that I gathered from my research, he was just a normal kid. The case bothered me for months, until one day, something in my head clicked. I let out a sigh of relief knowing it was nothing serious at all.
Turns out, the kid wasn't actually crazy, just upset at being constantly mistreated by the adults he lived with. When the mistreatment stopped, he stopped getting upset.
10. Factitious Disorder
When I was an intern, we had a 22-year-old man with persistent abdominal pain, all studies negative. His symptoms were unexplained. His mother was constantly at his bedside, and his medical history, which was extensive according to his mom, included multiple hospital stays with no definitive diagnosis. I noticed that he would frequently take ill after meals, which his mother brought from outside the hospital.
It eventually became clear that he was a victim of Munchausen by proxy. His mother was making him ill. I'd had a patient with Munchausen's when I was in medical school (she was injecting her own waste into her IV), so I was particularly tuned in. Both cases were very sad.
 Unspalsh
Unspalsh
11. My Old Mother
One of my favorites is when we had an 85-year-old man in for cellulitis or something, and everyone was documenting he was confused—in part because he kept talking about his mother; his mother was going to be so worried, he had to be discharged to take care of his mother etc. He became agitated and was actually getting ready to be dosed with Haldol because he was insistent he was going to leave to take care of his mother.
Note, the standard is to play along, tell the patient something like "Oh, we already called your mom, she knows you're here" that sort of thing, but he wasn't buying it. Finally, the nurse asks him if we can call his son to make sure the patient's mother is being taken care of (really, just to placate the patient), and the patient agrees. We call the son, the nurse explains the situation, and the son informs us that the patient's mother is indeed alive at the age of 101, but that he is staying in his father's house assisting in her care.
Poor patient was legitimately worried about his mom, and we all thought his infection (or just old age) was causing him to be confused!
12. Picking Up The Pieces
Nurse here. They don't teach you how to maintain honesty when your doctor skirts around a cancer diagnosis. I've had a few cases where a physician avoids questions and instead just tells the patients and families to wait and see what pathology shows. The doctor will then usually spend 30 seconds in the room giving vague information, then immediately leave me to pick up the pieces.
Patients often ask, “In your opinion, what did the doctor mean when he or she said this”? And my response is almost always straightforward—that when it presents like that, it usually means cancer. I want to be honest with them. I make sure to spend the next 30 minutes educating the patient and offering resources on what the next steps would be.
13. Mind Games
I cared for a patient who had gallbladder issues. About three days into his stay, he complained of bugs in his room. Then his tragic history came out. We weren’t aware that he was an alcoholic and withdrawal was setting in—his intake interview records simply listed: “Sometimes a few drinks after work”.
The patient threatened everyone who approached him, and he refused all meds including the sedatives which are used to treat withdrawals. Soon, he moved his roommate’s bed (with the roommate in it) to the room’s closed door and barricaded them both inside the room. The roommate was quite ill, had IVs running, and needed a breathing treatment.
I was really worried about both of them as that kind of withdrawal can be life-threatening. We were all totally clueless about how to deal with this. Security had started trying to break through the door, but that was only making the patient more agitated and more of a threat to his roommate.
We were a teaching hospital, so a psych resident was sent to the unit. The resident was young and I did not have much confidence in his ability to be useful. He ordered all personnel to be quiet and started to talk to the withdrawal patient through the door. Within 10 minutes, the patient had opened the door to the resident.
Within another 10 minutes, he let staff in to care for his roommate and accepted sedation for himself. Since then, I have great respect for the skill of a trained practitioner of psychology.
14. Sugar Pie Honey Bum
I did not know that a rectal prolapse can be treated with sugar. Depending on the extent of the prolapse, surgery is usually the only option. But one rudimentary method for a non-surgical repair is just putting sugar on it. Pouring sugar on it draws fluid out by simple principles of fluid dynamics—salt would also work, but that would be quite masochistic.
This shrinks the prolapse so it is easier to place back and also less painful for the patient. So, well, that is how I found myself opening a handful of sugar packets into a cup for a doctor at 2 am as an undergrad while working in an emergency room.
15. Spinal Tap
I am an anesthesiologist now, but was a doctor in charge of a small rural hospital in India about 20 years ago. An elderly lady was brought to the hospital by an irate husband who felt she was faking an illness. She would lie in a room all day with doors and windows shut and complained of a headache. She refused to do housework or look after the kids. Other doctors who had seen her before me had treated her for pain with no improvement.
I examined the patient; who complained of severe headaches and just wanted to lie down and refused to open her eyes. I admitted her to the hospital and performed CSF tap (A needle into the lumbar spine to get a sample of fluid surrounding the spinal cord). As expected, it was tinged yellow (Cerebro-spinal fluid should be clear). These days we have CT scans to diagnose sub-arachnoid hemorrhage (bleeding around the brain); but it was a difficult diagnosis once upon a time.
16. Wearing Your Heart On Your Sleeve
I diagnosed a little girl at birth who had Ectopia Cordis. It's a birth defect where the heart is located outside of the chest or thorax (yet it's still underneath the skin). It only happens to about 5-7 per one million live births. Warning, if you plan to search up "Ectopia Cordis," the images available may not be for the faint of heart.
17. The Worse Of Two Evils
We had a good case a few years ago. An otherwise healthy, 40-year-old migrant worker from Central America started coughing up blood intermittently. Everything suggested tuberculosis: History (they were from an area with lots of TB), chest x-ray looked like tuberculosis, illness script looked like tuberculosis...but his tests for it (sputum/quant gold) were all negative.
I decided to test his urine on a whim to rule out pulmonary-renal pathologies. Ding, ding, ding! Blood. Lots of blood. The patient never noticed it, and his kidney function was superb, so this was a tricky diagnosis. Turns out he had granulomatosis with polyangiitis (Wegner's). Kind of a sad story, because TB is largely curable, but with Wegner's he'll be on chemo for a very long time with this disease. I'm glad we caught it before irrevocable damage to his organs, though.
18. A Real Tear-Jerker
I'm not a doctor, but a pharmacy technician. About a year ago, a young woman who came in was very upset. She turned in a prescription for a bunch of anti-anxiety and anti-psychosis medications. All was going well until I realized we were out of one of them. I had to tell her that I needed to order it for the next day. She was OK with it at first, but then I saw the rage flooding her eyes.
I asked her if she was OK and she said yes, so I continued typing up the prescriptions. The next thing I knew, she began crying. She started telling me that she was just released from a psych ward and she had tried to harm herself a couple of weeks back. She rolled up her sleeves and her arms were covered in deep cuts. She began to ask me if I thought she would ever get re-accepted to nursing school.
Apparently, they kick you out if you get admitted to the hospital for psychological symptoms. I had no idea what to tell her except that I hoped she got in and that if she worked hard, they should give her a chance. I know this all may sound shallow, but I was not prepared for this. Nothing in pharmacy tech training told me how to react.
19. A Staple Food Source
I worked as a mental health tech to get through undergrad. A 15-year-old female in the adolescent ward claims to have swallowed a staple. Eh, but whatever, as I’m taking her down to x-ray, I tell her about the dime I swallowed when I was a kid. It happens. Well, turns out she underestimated the number of staples by around a hundred.
Every printout given by the therapists had been a swallowed staple. She had gotten staples from the other kids. The x-ray of her abdomen looked as if it were a weird staple-y snow globe. And yet, somehow, she was back to trying to take psych ward staples a week later. Never did figure out how they removed them all.
 Pexels
Pexels
20. A Parting Gift
Hospice pharmacist here. Pharmacy school never really prepared me for hospice care in general. Overall, I love my patients and their families, and I have become very close to them. Once, I had a patient who had a daughter in her mid-20s and we all loved to sit in his room with his family. They were so friendly and loving.
A few days into his stay, the patient asked me what I depended on my dad to tell me when I was younger. I told him that I needed my dad to educate me on a bunch of car stuff, money decisions; you know, basic dad things. A few days later, he gave his daughter a heartbreaking gift. It was a book of things she needed to know for when he was gone. I still think of that family to this day.
21. Things Fall Apart
Nurse here. You learn everything about the human body in school. Anatomically, physiologically, you know it all. However, you don't learn about the real emotional side of health care until you actually get out there. I had a patient who was depressed and got into a physical altercation. The county lockup brought him to our hospital for complaints of chest pain.
He was a sweet guy. He was a lawyer many years ago, and during a case where gangs were involved, the group he was prosecuting shot up his law office and his assistant didn't make it. He had a psychological break. He lost his law license and started hanging with the wrong crowd. He had no family, so he was basically all alone. The guy's lack of emotional stability resulted in him not being able to catch a break.
As it turned out, the chest pain was due to anxiety. His toxicology was clean, but he just couldn't get himself out of this hole. I really felt bad for him. He lost everything and struggled to get himself into a good place. I did everything I could to see if I could get him transferred to a behavioral unit so he could get the help he needed, but the admitting doctor said he didn't qualify.
I had to wake him up at three in the morning to tell him that he would be discharged and be going back behind bars. It was one of the hardest things I had to do. It was even harder than telling a family member their loved one wasn't going to make it and they should say goodbye.
22. If It Ain’t Broke, Don’t Break It
Patient here. One time, one of my nurses didn’t know how to give me my new medication. It was an Epi-Pen, and honestly, they're not that hard to administer, but she and the other nurses were playing around with it outside trying to figure it out. That's when the worst happened. They accidentally set it off—a $1,500 pen of allergy medication.
The doctor was NOT too pleased, and the nurse even tried to lie her way out of it, saying the pen was “defective”. My dad had to tell the doctor the truth. I was sitting there, half finding it hilarious, and half super angry because I’d been waiting for the medication for four days and then had to wait even longer.
23. Words Of Wisdom
In hospice, if you whisper "It's OK, you can go. I will take care of your family" to someone who is "active" (actively passing), they pass a lot faster and more peacefully. Hugging the primary caregivers and telling them "You did such a good job" can also really help them positively process what’s happening.
24. Cat’s Cradle
When you have to euthanize a 91-year-old woman’s ancient cat who belonged to her husband; then, when you set the cat on the hospital blanket, you ask the sweet old woman who lost her husband and daughter in the same month, “Would you like your blanket back”? And she answers with tears in her eyes, “I just want my family back”. No, it doesn’t get easier.
25. You Tried, You Failed
“She’s depressed because of work”. No, ma’am, she has schizophrenia. “She has a borderline personality disorder”. Did you mean, “She is female and insisting there is something wrong when you want to write her off”? Also, what she has is a brain tumor, so thanks for playing, goodbye. “He has anxiety”. Nope, he has OCD, I’m not sure how you missed it because it’s not subtle.
There’s a reason I got the heck out of that job.
26. Growing White
Menkes syndrome related to hair texture. I was called to see a 3-month-old boy with hard-to-control seizures. His most remarkable exam finding was his hair: he had been born with a full head of black hair (he was Hispanic), but at the time I saw him, the first 3-5 mm of each hair shaft was nearly white, with an abrupt color change, still black on the tips. The hair was a giveaway for this disorder, almost no need for confirmatory testing, but the admitting team had already ordered whole exome sequencing.
This was not a fun and exciting diagnosis to make, more a sinking feeling upon discovery of the hair (neurodegenerative disorder due to a defect in copper metabolism that is irreversible once symptoms appear), but it was interesting to see at that transitional stage. I had only seen older boys with Menkes before, once the hair was already pale and brittle all over. Usually the hair has changed long before the diagnosis is made.
27. Toilet Training
I took care of a young man with a wound in his abdomen. He had an ostomy bag to collect his bodily waste for a while. When they finally removed it, he was so nervous because he hadn’t pooped in so long. Then, one day, his call light went off in his room.
I came in and he said, “Go look in the toilet, you’re never going to believe this”! I went in and there was his poop in the toilet! His first solid poop I had seen in over a year! I walked out and gave him the biggest hug. He was so proud of his poop. I literally had tears in my eyes. Nursing school never prepared me for crying outside of a patient’s room because I was so happy they pooped.
28. A Real Head-Scratcher
This one was fun: a patient in the ER received a standard urine substance screen. The test came back positive for ethanol, but the patient insisted he never drank a drop. The test was then repeated. Positive. The patient got very upset. He swore he did not drink. So we drew a blood test. That's when things got weird.
The results came back negative. We checked everything we could think of. Did we have the right urine? The right blood? It should be impossible to test positive on urine and negative on blood. Meanwhile, I finished his regular urinalysis. He had a high white blood cell count and really high glucose. Elevated white cells usually require microscope inspection because it could indicate an infection.
I looked and it was loaded with yeast. That’s when it all made sense to me. The man was obviously diabetic and had high sugar in his urine, along with a yeast infection in the bladder. See, the yeast was fermenting the sugar into ethanol in his bladder. He then became known as 'The Man Who Peed Beer'.
29. Getting The Stiff
When my mom was fresh out of nursing school in the 1980s, she got a job at a hospital that had a high concentration of geriatric patients. One particularly frail man took out his dentures before sleeping, then passed in the night during her shift. His cheeks were so alarmingly sunken in that my mom and another nurse tried to replace the dentures back in his mouth so as not to horrify the family.
Unfortunately, the rigor mortis had already started to set in. She said nursing school definitely didn’t prepare her for that nightmare.
30. Gimme More
When I was in labor with my first son, the anesthesiologist gave me an epidural, as requested. However, things quickly got complicated. I was rushed out to have an emergency C-section. They got me prepped for it in less than five minutes and started cutting. I could feel everything and I started screaming. At first, they got kind of eye-rolly. Then, the doctor let out a "whoops". They forgot to up the epidural for a C-section.
31. How To Save A Life
I did chest compressions on a daughter’s mother while the girl stood at the head of the bed, pleading that I save her mother’s life. I’ve had some form of medical training since I was 16, but using it so often in a hospital setting makes you less empathetic. I’m also a male nurse if it makes any difference. I didn’t expect to get the feels after such a critical moment in a family’s life.
The mother survived. I definitely broke most of the bones in her chest, though.
32. A Bonding Experience
When I worked in assisted living, I had a gentleman on hospice. He was a nice guy and was as cooperative as could be. 30 minutes before leaving one day, I was doing my rounds and making sure everyone was getting dressed. This patient needed assistance, so I started doing his routine. All of a sudden, he said he needed to poop.
I asked him if he could make it to the toilet. We tried to make it, but it was in vain. We ended up in the shower just spraying every time he passed a movement because it was the easiest solution. It was absolutely one of the worst things I’ve dealt with in my life. It seemed like it would never end. I ended up getting him cleaned up and in his freshly cleaned wheelchair.
Meanwhile, I stripped his bedding and the rest of the linen casualties that we’d amassed during this adventure. I tucked him into his fresh bed and told him I’d see him that night. My co-worker had the absolute balls to ask where the heck had I been while I carried all of his linen to the laundry. I told her to bug off because I had just handled the poo explosion of my nightmares completely solo.
Still, he and I became quite good friends after that. That kind of thing will bring two people together.
33. Rare and Terrible
Wolman Disease. A genetic disease that affects about 1/200,000 kids, terrible outcome. It leads to calcification of the adrenal glands, which is how I picked it up on a chest x-ray on-call (I'm a radiologist). The kid had failure to thrive and a big spleen so I brought it up. He got further testing which confirmed the diagnosis.
Bottom line, don't forget to look at the adrenals or ribs on peds x-rays!
34. The Cleanse
I had a patient with a terrible infection at an injection site. I watched in fascination, horror, and disgust as the surgeon squeezed the patient's arm and thick pus slowly squirted out of the incision. It was like squeezing a tube of toothpaste. To be honest, I found it to be really satisfying because here was this nasty infection that could really harm this person and it was being cleaned out. I could feel the person feeling better as it was being cleaned.
35. Dangerous Liaisons
I’ve learned that people will literally stick ANYTHING up their butt and the operating crew will get called out on a beautiful weekend day because of it. Every. Single. Time. Then, as they are going up to the floor to wheel the patient down for surgery, the patient will invariably greet them with, “Hi, I’m the village idiot”. Yes...yes you are, and you just bought yourself a permanent colostomy bag.
36. A Quick Diagnosis
I once saw a child with mosaic trisomy 8. It was a complete mystery why he had speech apraxia, and the geneticist I was working with took one look at his feet, saw that they had super deep creases lengthwise, and ordered a karyotype with mosaic trisomy 8 in mind. Sure enough, he was right. I was amazed how spot-on he was predicting that.
37. Flippant Flipping
I didn't diagnose it, but I have a patient with primary Ciliary Dyskinesia with Situs Inversus, aka Kartagener syndrome. The cilia in the body don't move well, and this mainly affects the respiratory cilia/lungs, although it also causes infertility, related to the cilia inside the fallopian tubes and the sperm tails not working well.
Situs Inversus is when the organs inside the thorax are mirror images of normal, the heart is on the right side instead of the left, etc. I was looking over this patient's old medical records and one of the radiology reads of a chest x-ray said, "There has been interval development of dextrocardia. Since this is physiologically impossible, the film has been flipped".
Probably the original film the radiologist had been comparing to had been incorrectly flipped to look "normal," maybe by someone who assumed there had been an error. Another chest x-ray report just read: "The film has been flipped" and then went onto the rest of the interpretation.
 Unsplash
Unsplash
38. Ignoring The Issue
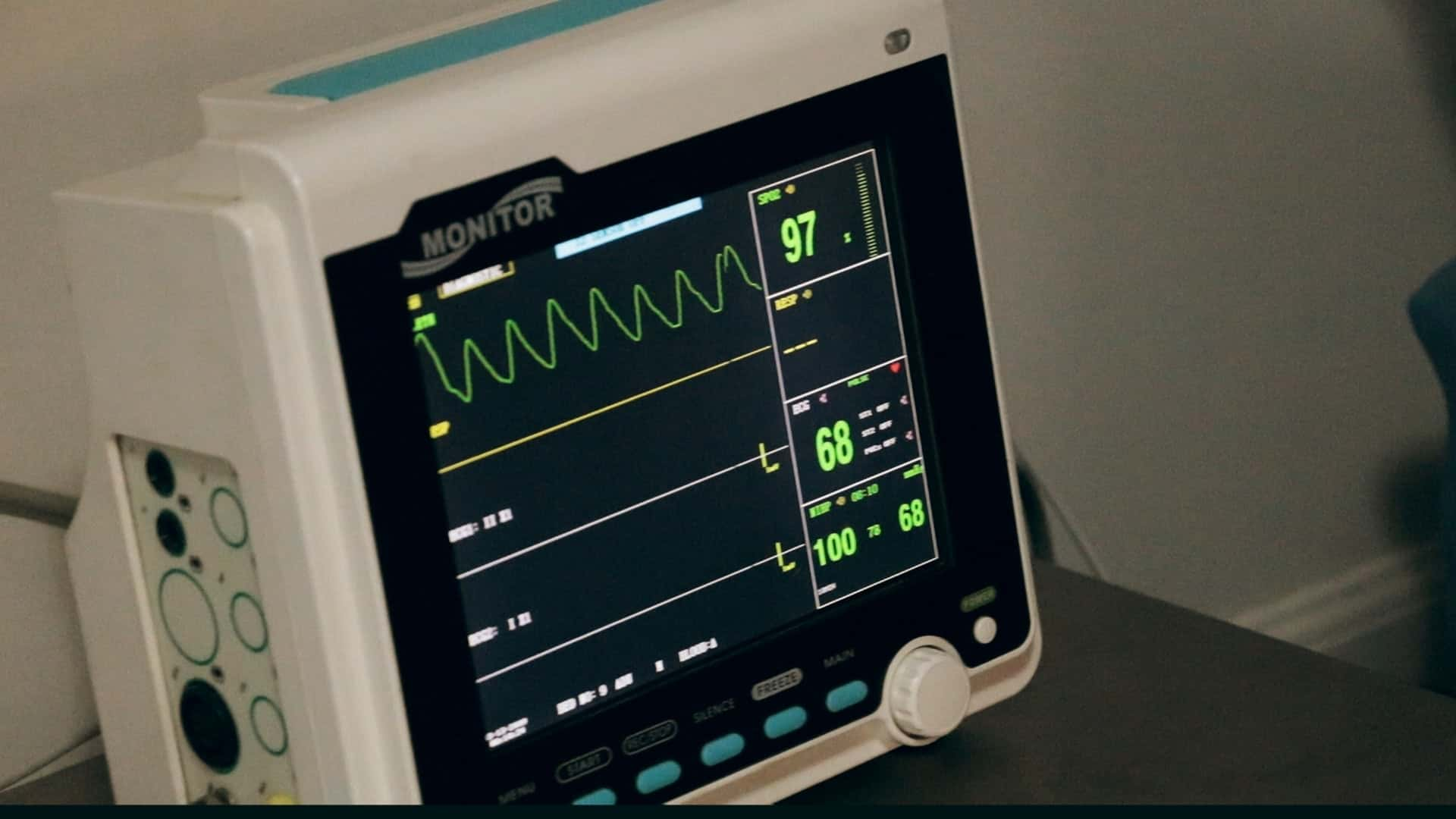
I'm an anesthesiologist. This happened when I was a resident. It changed me for life. We had a 29-year-old male in for finger surgery. We had an uneventful induction maintained on Sevoflurane. Within 20 minutes we started to have rising ETco2. I called my attending after trying to hyperventilate the patient (She was a young Harvard-trained peds anesthesiologist).
She comes in and asks me what I think is going on. I tell her things seemed strange. She tells me to chill. Five minutes later, the ETco2 is over 100 and I'm freaking out! I call her and tell her this is MALIGNANT HYPERTHERMIA (easily fatal reaction to certain anesthetics caused by congenital aberrant sarcoplasmic reticulum receptors).
She says that I'm being ridiculous when I tell her I'm afraid this is the real deal. My pages get ignored by her. The patient’s temperature starts to rise. I'm bugging out and call the board runner (supervising Anesthesiologist for all the operating rooms). He's old. He knows me well and trusts me. Comes in, looks at the monitor—and his face went white.
Needless to say, we save the patient after many dozens of vials of Dantrolene. Six months later I'm made to do an M&M and the young Harvard attending insinuates I did something wrong in front of the department. Most of the rest of them come to my aide. She leaves the job shortly thereafter. I will soon be at her fellowship.
Weird.
 Flickr
Flickr
39. On A Hunch
ED referred a guy to me who had a platelet count of 2. The guy looked bloody sick with abdominal pain, petechial rash, feverish, diaphoretic, and he was a bit confused and drowsy too. I talked to my boss who said to give him prednisolone and he'd see him tomorrow, but I was convinced this guy had a really rare condition called TTP (Thrombotic Thrombocytopenic Purpura) and so I called the major hospital in my area and sent him to their ICU for a procedure called plasma exchange.
I ordered a test called ADAMTS13 to prove the condition, and still have a paper copy of the result (he had none of this chemical) because it's the best diagnosis I've ever made, it helped save his life!
40. More Than Meets The Eye
As a fourth year during my rotations, I noticed my patient had a vertical subluxation of her crystalline lens during a dilated eye examination. The part of the eye that develops a cataract later on in life was shifted significantly up. She had severe myopia and astigmatism (-14.00 - 5.00 x 180 OU), and her 6'1" tall body along with disfigured teeth led me to believe she had Marfan's Syndrome.
She had never heard of it, never seen a cardiologist, etc. A few lab tests confirmed. She can live a normal life; she just needs some meds and education. She had very long fingers that jumped out at me and braces on her teeth. As an optometrist, I focus on glasses and contacts, but I see (no pun intended) and treat an unbelievable number of systemic diseases that manifest in the eye or retina.
41. Hard To Miss
A woman came in with severe opiate withdrawal and some shortness of breath. Because she was so insistent about how miserable she was, everyone sort of wrote her off as drug-seeking. The morning I rounded on her, I decided to do a thorough physical exam. Lo and behold, she has a hard non-mobile clavicular lymph node...it was so big that it was impossible to miss if you just did the exam.
Immediately we got a chest x-ray and then a CT scan. There was a perihilar mass. After a biopsy, we learned it was small cell carcinoma (lung cancer).
42. No Face
Baby born without a nose and with non-functioning eyes. Diagnosed with Bosma Syndrome. It was kind of crazy, I saw the baby a few months later and it was doing fine. Children with Bosma Syndrome grow up without any cognitive disabilities, it's very interesting.
 Pexels
Pexels
43. Pill Problem
I'm not sure if this counts as a rare diagnosis but it was a neat one. This fellow was at dinner with his wife and some friends when "all of a sudden" he slumped forward into his entree and went unconscious. I saw him as a hospitalist in the IMCU. Despite being unconscious, his labs and vitals were all stable and he appears to be adequately protecting his airway.
The wife was initially understandably distraught and not able to offer the best of histories, but as the patient gradually began to wake up, I was able to put together a few facts. The patient had pancreatic insufficiency and thus needed to take six pills with pancreatic enzymes before each meal. He also had a prescription for Ambien. They were both white pills...you can figure out the rest. He recovered fully without any long-term effects.
44. Thar She Blows
I was NOT prepared for the day a patient exploded in surgery and splattered all over the entire operating team. Basically, a watermelon-sized tumor was being removed from the patient. It turned out, the tumor was more of a giant cyst. The surgeon didn’t open up the belly wide enough to facilitate the thing, so imagine someone trying to dig out a giant water balloon from an eight-inch incision with their hands.
The pressure on the tumor caused it to erupt out and upwards, spraying its contents on everyone and everything in the room. On the positive side, this made the removal of the thing A LOT easier. I do recall a lot of people screaming when it happened though. The patient came out fine!
45. Tearing It Up
I watched one of the biggest screw-ups ever. My sister is very tall, very thin, and very fit. She was in pre-season for her WNBL season, so she had been running medium distances. Suddenly, she had a sudden sharp pain in the left side of her chest, along with radiating arm pain and shortness of breath. She called an ambulance and was rushed to the hospital.
They did all the tests and determined there had been no heart attack. They said she simply tore a muscle and sent her home. Welp, a week later, she was still in pain and she swore she heard a hissing sound in her chest. She saw our family doctor. He listened to her chest while she breathed in and out. He then said, "You've torn your lung”.
She was the perfect candidate for a torn lung. Tall, thin, fit. Her doctor was amazed the hospital didn't hear the tear. How do you miss a torn lung in a perfect candidate for a torn lung?
46. School’s Out
My grandmother was a school nurse at an elementary school. They were letting the kids out for the day, and all of the kids were waiting outside. One little boy's mom came to pick him up. As she was walking up to the building, she began to have a heart attack. My grandmother began CPR and sent someone to get the defibrillator. She also told another teacher to call 9-1-1.
The woman passed before the ambulance arrived. I don't think twice her time in medical school could've prepared her for that.
47. Just Say No
Today I took care of a man who believed he had been bitten on the abdomen by a baby rattlesnake that had fallen out of his ceiling vent, crawled up his abdomen under his skin, up his throat, and was currently coiled and rattling in his brain. Diagnosis: methamphetamines. Just say no.
 Flickr
Flickr
Shutterstock
48. Dr. Google
Probably Stiff Person Syndrome. Technically it was paraneoplastic antibodies causing a case of mild stiff person-like syndrome, but it was basically a lady who had glutamic acid decarboxylase antibodies which caused her to be really stiff. How'd I figure it out? Well, she was really stiff and it was very odd. I was out of ideas and literally googled "stiff person" and got the result of a disease I'd probably heard mentioned in passing in med school but is so rare you forget about it: Stiff Person Syndrome.
Yes, it's real. I thought it was a joke at first—but it's all too real. Ordered the test, it was positive. Later, after more research, I learned that you can have similar antibodies and symptoms with paraneoplastic syndromes, so I did a scan, and found a lung tumor. Boom. SPS is really rare. Paraneoplastic syndromes are less rare. She was somewhere in the middle.
49. Cradle To The Grave
When my wife started out as a fully-fledged registered nurse, her first job was in an aged care facility. She said the hardest part was getting used to working with people with dementia and the things that they'd do. For example, she had residents who would eat their own poop—she had to go home early after that one because she was so sick for the rest of the day.
There was another resident who once walked down the hallway with poop in her hands. She had no idea what it was or how it got there. They had to remove the Christmas tree from the dementia ward after another resident peed on it. But those aren't even the worst cases. The toughest ones to handle, however, were the violent or aggressive residents; many of whom were (according to their families) sweet, loving people before they got sick.
She also had one resident who apparently was an angry jerk before he got dementia but then turned into a kind, lovely old man, so I guess it can go both ways. In a way, you sort of understand them though. If you have no idea who anyone is or what is going on, it would be very distressing if a random stranger takes your clothes off against your will every day and then puts you under a shower.
It was also really distressing for her to help residents who couldn't remember that their spouses had passed. They would ask every 20 minutes where their husband or wife was because they couldn't find them. Apparently, nurses learn quickly that the easiest answer is just to lie. “She's just gone to the pharmacy to get some medicine, she'll be back soon”.
One family tried to be helpful by making a very beautiful photo album for their grandpa showing a lot of photos of him and his wife together. They finished the book with photos of him at her funeral to help him remember that she had gone. The only problem is, things like that tend to just make people re-live losing their loved one over and over again each day, so the nurses found it easier to just lie.
So in short, many aged care facilities are terrible; but if you can find a good one with good nurses and good staff, your loved ones will be treated extremely well with people who love and care for them.
50. A Tale Of Two Families
Working in the ICU, I see mortality all the time and have essentially become numb to it. I've also seen the very best and worst of the process demonstrated by family members. The best case: I had a family whose father had stage 4 (end-stage) liver cancer with metastasis to the lungs and the pancreas.
He was experiencing horrible pain but was he was also utterly exhausted from his years of chemo and treatment. He finally said enough was enough and made the decision to move to comfort care. For those who don't know, comfort care is when we withdraw any form of invasive treatment from a patient. We switch them to primarily pain control only.
This one patient, let's call him Bill, through a quiet whisper, made the decision to go to comfort care. He wanted us to contact his family to come and see him. The staff agreed and they called his family who were able to make the trip. One by one, the sons, daughters, grandkids, and even the great-grandkids went into the room on their own to say their goodbyes.
Before he passed, Bill wanted to have a glass of merlot with his family. So Bill’s son drove as fast as he could to a nearby store and bought the cheapest boxed stuff he could find. Together, the family sipped on a cheap glass and enjoyed the presence and stories of their beloved Bill. A short while after, through tears, Bill's family watched him slowly and peacefully slip away.
What truly stuck with me during this event was how the family acted during Bill’s passing. They weren't saying, "Come on Bill! You're gonna beat this! Keep fighting”! etc. Instead, they encouraged him to relax, saying, "It's okay Bill, we love you so much. You don't have to keep fighting anymore". They all knew his body was failing, and so did Bill.
Before he passed, Bill’s whole family was present and enjoyed being with him until the very end. While there was mourning, and rightfully so, there was also a sense of joy and peace. Now the bad: We had a patient who also had end-stage cancer of the lungs with metastasis to the liver and bones. We will call her Jen.
Jen was in constant, excruciating pain. The only audible noise she'd make was a moan during each expiration. Due to her condition, Jen required aggressive blood pressure support and breathing assistance using a mask. Her family was adamant about the aggressive treatment of the patient, thinking that her condition could be fixed somehow.
Even after an extensive explanation of Jen’s condition, the family was still certain they wanted to treat her. So we did. What I remember is how the family, even after being told the patient was dying and that nothing we could do was going to help, was blinded by their expectations.
For whatever reason, they couldn't comprehend that end-stage cancer is not curable and that specifically bone and liver cancer are going to have extensive effects on the rest of the body. Even though Jen, the patient, was moaning in agony, the family insisted on continuing treatment. Because Jen was not making comprehensible sentences, we had to follow the family’s direction.
The staff could not look the family in the eyes because each one of us believed that what the family was doing was atrocious and inhumane. Eventually, Jen passed and her family was still upset with staff for not making her better. The family members were yelling at each other, criticizing each other for not doing this or that.
Instead of being at peace, all we saw was anger. I was never taught in school how to handle either one of those family dynamics. Nobody explained how to navigate difficult conversations in a professional and honest way. I see mortality every day and have come to realize that even though there is grief, there can also be happiness.
51. Let It Go
On my first day on a new ward, an older woman rang the buzzer in the bathroom. Me being keen to impress, I ran straight to her. I was confronted with a wall of smell and what looked like an explosion of poop...everywhere. Up the walls, just everywhere. Turns out, she didn't think she needed her laxatives the past few days, so she hid them.
The doctors, wondering why they weren't working, increased her dose...then she took them all at once when she felt bunged up. Oh, and she had also been eating an abundance of fruit. I had to use several disposable mops to reach parts of the wall. Honestly, I've never seen anything like it before or since. Luckily, I work in neonatal now.
52. His Cup Spilleth Over
I was still in nursing school at the time this happened and I worked as a nurse’s aide overnights. I had been taking care of this really lovely old guy, and we had some great conversations. He was “with it” and doing well. In the morning, he had told me that he hadn’t slept well and was really looking forward to getting coffee from the cafeteria people.
Later that day, his call light went off and I went to check on him. When I opened the door, he said, “I think I spilled my coffee”. When I realized what it really was, the blood drained from my face. I turned on the light and there was poop everywhere. All over him, all over the walls, a bit on the ceiling, all over the bed, and on the floor. He was holding his cup of coffee, which also had poop all over it, and he was just looking at me.
53. Sic Transit Gloria
Actually, pretty much everything I saw and did when working in oncology was new to me after medical school. It was the most amazing, rewarding, messed up, and emotional thing I've ever done. One day, I was leaving work for two weeks of holidays and said goodbye to my patient who I'd been looking after for the last week.
Both of us knew it was the last time we would see each other, as he wouldn't last two weeks. I can't even explain how much it affected me. He didn't want to pass and he was an absolute legend. That was four years ago. I think of him all the time; he was stopping treatment a few days after my holidays and going home to have a party with his buddies from the soccer club.
54. One In A Million
The morning report was a good one today. We had a 59-year-old male come in with lower leg swelling. Within 3 days he becomes confused, febrile, and stiff. We put him in the ICU, thinking he had meningitis and got some CSF cultures and started antibiotics. Two days later, the cultures were still negative and he wasn't improving.
His wife then says this whole event seems similar to her husband’s (the patient’s) mom. She had Creutzfeldt-Jacob disease and passed from it. It's a 1 in a million (literally) diagnosis and our tests are still coming back for it. Really rare case most doctors will never see.
 Pexels
Pexels
55. One Flew Over The Cuckoo’s Nest
I was a psych nurse for nearly two years, and honestly, we learn very little about psychology in school. The clinical lessons were basically useless, so there was a lot I had to learn as I went...like how to stay calm when you’re cutting a pillowcase off someone’s neck that they tried to hang themselves with, or how to deal with a psychotic teenager who’s bigger than you punching holes in the drywall and then using the pieces as projectiles.
Or what to do when you walk into the dark day room at 3 am to find your patient perched on top of the giant TV near the ceiling like he’s schizophrenic Batman. Yeah, there was never a dull day.
56. All Eyes On Me
Medical school didn’t teach me how to put a fake eye back in. A patient came in from a not-so-nice nursing home with a multitude of problems, one of which was a disgusting, draining fake eye that had to be removed for treatment. Upon discharge, we had to put it back in. Simple enough…or so we thought. We had no idea how to do it and struggled to figure it out.
I suppose that is why the nursing home staff never took it out to clean it in the first place. This was decades ago, though. Fake eye technology is probably much better today.
57. Breathe Easy
Years ago, I had a respiratory infection that kicked my asthma into overdrive. At the time, I didn’t have a primary care physician because I didn’t see the point, so I’d just go to urgent care for everything. Despite my peak flow meter reading being at 50% and telling the urgent care doctor that I’d had to sleep sitting up the night before—a huge red flag that the patient isn’t properly oxygenating—it did not go my way.
When I asked for a breathing treatment, the doctor said no. He simply said, “I’m sending you home with prednisone since your O2 is at 97%”. Note that our bodies are really good at compensating for bad lungs, so if an asthmatic has a low O2 saturation, they should’ve gone to the emergency department an hour ago. I eventually did get a primary care physician and I know now why I have one.
I eventually told my regular doctor about that urgent care doctor who wouldn’t give me a breathing treatment, and my doctor got SO angry. It made me feel very vindicated. And as a postscript, I had to go back to that urgent care the next day, where a different doctor gave me a breathing treatment because he wasn’t a total idiot.
58. Jack Of All Trades, Indeed
It was my first year out of my family practice residency. The specialists like to sneeringly refer to us as jacks-of-all-trades and masters of none. Anyway, I was on call from the ER, and a normally unshakable ER doctor was beside himself. He had a very pre-term mom in active labor and the fog outside that day prevented us from flying her out to a well-equipped hospital.
He was the only ER doctor, and the transferring facility wouldn't take her into transport without a physician on board, so they called me in. En route, I was trying to coach her to breathe through the contractions. Then disaster struck. She felt something coming out—it was the baby's foot. We were in the back of an ambulance when this happened.
We delivered the baby about a minute or two out of the hospital. When we got there, they were expecting a mom in pre-term labor, not a micro-preemie. One nurse met us in the ambulance bay, took a look at me holding the baby with a blanket and oxygen, and said, “Follow me”. We ran through the hospital and turned on an incubator.
The pediatric doctor wasn't present at that moment and the baby's heart rate was low, so I proceeded to intubate her. That was 12 years ago. She survived and is doing great. I wrote my program director at 4 am that morning when I got back home thanking him for all the training. I think I used 100% of my training that night, and it still didn’t prepare me for everything.
59. A Rash Of Problems
I had a small rash that wouldn't go away, so I went to see the doctor after a long while of hoping that it would just disappear on its own. He said it was ringworm and gave me an antifungal, but the rash got worse. I went back and he gave me an even stronger antifungal. Still, the rash spread, and this time it was all down my arms. I went back to the doctor to get a referral to a dermatologist.
The dermatologist took one look at the rash and said, "That is contact dermatitis". I had changed soaps and it irritated my skin, giving me a little rash. The doctor's stupid antifungals, in the meanwhile, were making my skin go crazy. I just stopped using soap for like a week and it was fine, but I had skin discoloration for like a year.
60. Bedside Manner
The first time I had to tell someone their loved one didn't make it, I was not ready. Though they covered the basics of it at medical school, no one really told us how to break the bad news to someone. No one told us how impotent we'd feel doing it, or the fact that we wouldn't be able to answer their panicked questions...or what it'll be like knowing that there's nothing we can say to family members that will truly bring comfort.
There’s also nothing on how shocked or even angry you'll be when some people don't really care about their mom going downhill, or how ashamed you might feel when you look back and realize that you're becoming numb to it all yourself. Yeah, you probably had to click through some presentation on the five stages of grief at some point and listen to a generic lecture on what NOT to say, but until you've stumbled through it a few times, you're winging it, and probably poorly.
61. Young, Not Dumb
I have Crohn’s disease. Because of it, I was severely malnourished when I went through puberty, so I'm a bit shorter than doctors predicted I would be and I look very young for my age. In my late teens, I would get really awful flare-ups of Crohn's and would have to go to the ER. About 75% of the time when I went to the ER in my town, they immediately assumed I was just faking it.
Usually, after one of my parents dropped me off at the door and went to park the car, I would have to argue with the front desk ladies and the security guard, since they were always skeptical. They would tell me, "Oh I'm sure you're fine, why don't you head on home"? It would take my parents coming in and yelling at them to shut them up.
I understand how scary it feels to be in so much pain and having no one believe you. I have a running theory about ageism when it comes to pain management in hospitals. I remember one time I was once admitted and, by coincidence, my roommate was a 40-year-old guy with the exact same diagnosis as me. I got to see the huge difference in care between us.
At one point, the head nurse pulled all my pain medication from me and actually said to me, "When I'm here, the pills stop". My roommate got great treatment the whole time, though. Rest assured, after this stay, my parents had made many calls to supervisors, department heads, and people who dealt with lawsuits to severely complain about my treatment.
I was very sick at the time, so I was really in no condition to fight for myself.
62. Poker Face
Sonographers have to keep a poker face a lot of times when they see something very alarming or sad on the screen. Luckily, most people have no idea what they are looking at, but they’re not allowed to give any results to patients since doctors deliver the bad news. They simply have to stay neutral. A couple of months ago, I had an ultrasound done and was talking with the sonographer about how happy I was to be having a baby.
I’ve lost many people this year and I needed some good to happen. Then I saw her face, and my blood ran cold. It wasn’t super obvious, but I knew. My baby’s heart wasn’t beating, and I didn’t see any movement. She pulled away and told me that a doctor would call me that day. It was awful for me. I remember calling my doctor a few times that day because I wanted to know those results right away.
When I finally got it, I broke down. But I still feel really awful for her. She didn’t say much, but I could really see her heartbreak too. Their job is a lot harder than most people would imagine.
63. There’s A Butt
The complaint in the man’s file was rectal pain. I immediately thought hemorrhoid, abscess, or a fissure. When I saw Mr. Rectal Pain, he told me he had pain down there but had no other symptoms. I got to the examining part it was normal looking. At that point, I had to proceed with a rectal exam. The result made my jaw drop.
I digitally examined him and he instantly said, “Ow, there’s something sharp in there”. Out came a fishbone. It was big too, like two or three centimeters long. I asked the patient about it and he was like, “Oh, I had red snapper a few nights ago”. I put the fishbone into a specimen cup and started parading through the emergency department showing everyone what I just “fished" out of some guy's butt. Oh, and there’s a coda to this tale.
I told this story to my colleague and he proceeded to tell me how in his residency they did rectal exams on all trauma patients. One time, one of his fellow residents went to perform one and the patient said the exact same phrase: “Ow, there’s something sharp in there”. But instead of a fishbone, it was a hypodermic needle. You can’t make this stuff up.
64. Dr. Jekyll And Mr. Hyde
Some people talk while under anesthesia. Some people even scream. Honestly, it gets so bad sometimes that I used to go home in tears, especially after treating very vocal patients. The only thing that helped was when patients would wake up and tell us, “Thank you so much. That went so fast”. Post-operative checks a week later when I could see the patients were still doing well helped too.
I remember asking the doctor over and over when I first started, “Are you sure they’re under, are you sure they’re numb”? Now, after a few years’ experience, I understand how much local anesthetic he used. The patients were likely numb for a few hours post-treatment.
65. Against All Odds
Five years ago, I spent six months working in a small rural Zambian hospital in the medical ward as part of a volunteer/outreach program. I have done mostly family medicine, and some surgery in my early days, but decided to mix life up a bit. The hospital was a typical third world—a few basic medications, rudimentary clinical tools, a small lab on site which was usually broken.
No resuscitation tools whatsoever. HIV, TB, and malaria were rife—it would not be uncommon to encounter a loss per day despite our best efforts. On one of my first days there an unconscious person was carried in by a mob of locals. I could smell him before I saw him. He had been in a house fire and his skin was cooked—completely black around his chest, face, and over his legs.
He was still breathing on his own and maintaining his airway but we had no doubt he had inhaled a lot of smoke. With no way to intubate or provide the oxygen we merely had to hope that he didn’t swell up and close off and deal with the rest of the burns while he was unconscious. Two colleagues who worked in the hospital came over urgently.
We all kept our cool externally and got the nurses to translate to the man’s family that we were going to do everything we could to get him better. In reality, all three of us knew his chances at survival were in the single-digit percentages. We decided that due to the extent of his burns we were going to have to do an escharotomy (cutting the burned skin to prevent it from contracting and stopping him from breathing).
Turns out I had the most surgical experience so despite having never done one before I gave it a go, hoping for the best. We got an IV into a neck vein and got fluids going. The local nurses dressed his burns. We gave him whatever pain relief we had. He was unconscious for a couple of days but eventually came to.
Each day we were expecting his kidneys to pack up but to our surprise, gradually he got better. He was with us for just over four months recovering. He came out severely scarred but he had beaten the odds and survived.
 Pexels
Pexels
66. A Twist Of Fate
Sometimes, even when you do everything you're told to do, tragedy happens. You are going to have an elderly patient who you know won't make it, but there is little you can do about it other than lessen the damage. There is going to be a patient’s family member you get a little too close to and you will feel hurt when they blame you for something.
You will trust your superiors and possibly get thrown under the bus for it. I had an instance where I had a new patient who arrived on my day off. The nurse gave me a very quick report about him when I came back and I was told that although he would be a little resistant, he wasn't combative. In fact, he was purposefully placed with me because I was pretty calm and often chatted with my patients.
We were short-staffed, as always. I had another nurse assisting me to transfer him, but the nurse had to leave to get an oxygen canister for him…and she never made it back. My patient got a little restless as we were waiting. I couldn't move him in his wheelchair as he was hooked up to a mounted canister, and I also couldn't leave him alone.
While I was standing there, he pulled a shocking move on me. I wound up getting punched in the eye without any warning. My glasses broke and I was stunned. I pulled the call light, but...nothing. I looked out the door but there was nobody there. I wound up using a phone to call the front desk and beg the nurse to come down because he hit me and I didn't want to be there alone.
It still took her 15 minutes. At that time, I started to realize something was seriously wrong. At some point, I went to the doctor myself. It turned out, I had a concussion, a minor cartilage break in my nose, plus a black eye and vision issues. It’s been a few months now and I've lost central vision in that eye and I have started getting spots and floaters in the opposite eye.
They're going to probably take my license soon. I’ve seen several doctors and specialists who are at a loss and don't think they can do anything. I've been told surgery wouldn't do anything because the rods and cones are pretty much gone in that eye. Plus, I have migraines daily now. I wanted to go to school to be a nurse. I'm not even 30 and now I have to give up on my dream.
Protect yourself. Little things can change your entire life.
67. A Bad Prognosis
As a third-year medical student, I had a patient come in with four years of worsening balance issues and garbled speech. She had gotten a crazy work up at an outside hospital system with every sort of imaging possible, biopsies of random sites, and a number of very expensive tests. She was at our university hospital for the first time.
When I first entered the room, I reached out to shake her hand, and from her wheelchair she had to raise her head at me because she couldn't look up with her eyes. This was the first red flag. I also asked her if she had the sensation where one of her limbs would move without her controlling it, and she said yes, suggesting something called Alien Limb Phenomenon.
I diagnosed her with Progressive Supranuclear Palsy with features of Corticobasal Degeneration, a very rare disease on the spectrum of Parkinson's plus syndromes, and my supervisors agreed. Unfortunately, it was a bad prognosis, but the family was consoled by the fact that at least they had a name for what was happening.
68. It Hits The Fan
From the reverse perspective, my family tends to entertain the ER with emergencies nobody expects. One time, I gave myself a concussion and whiplash—from a ceiling fan. I broke it on my skull, knocked myself out for like 30 seconds, and then had migraines nonstop for eight days. Surprise, ER! So many people in the ER kept stopping by to ask me my story and laugh about it like, "Now I've seen everything"!
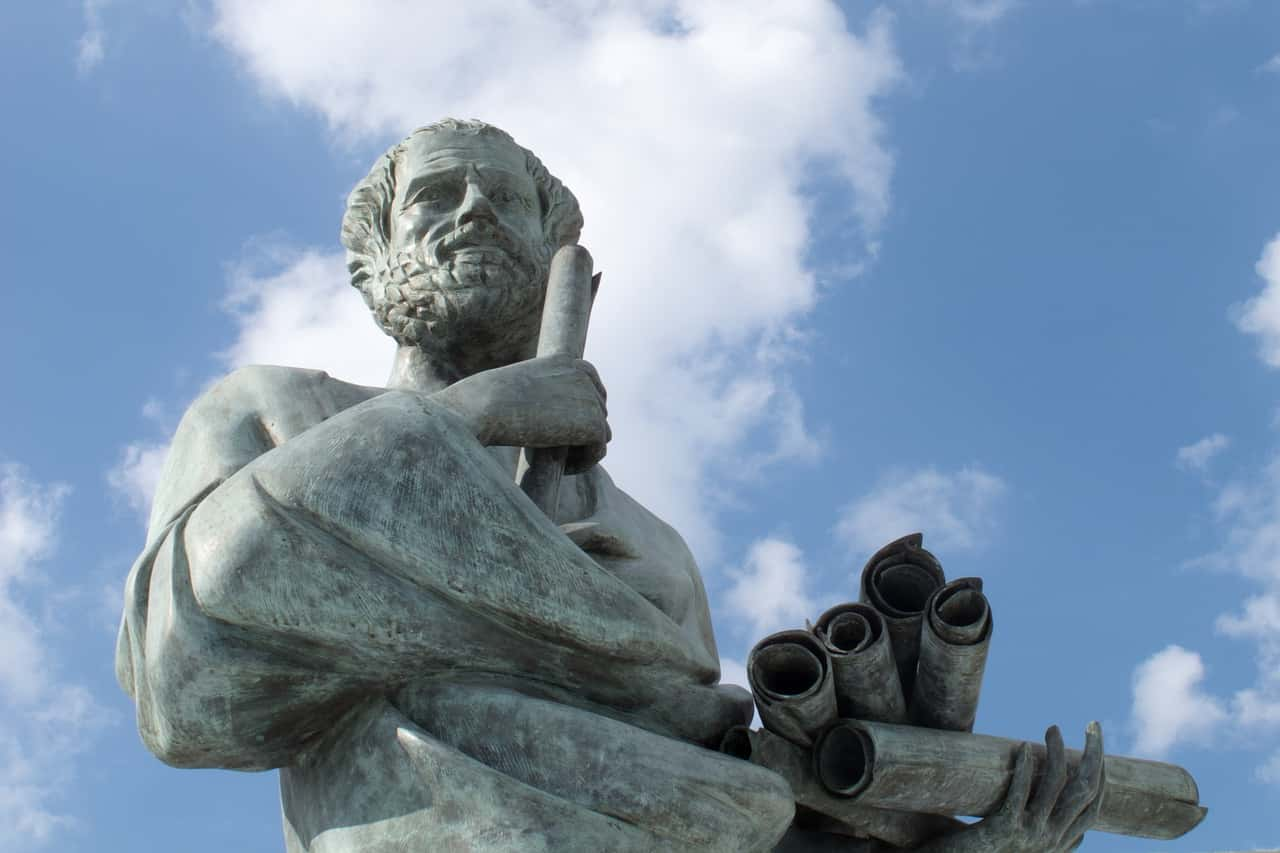
69. Socrates’ Demise
We had a young fellow come in who worked as a landscaper. He showed up in the ER with severe GI distress. The diagnosis was almost entirely from history. Apparently, he forgot to bring lunch so decided to munch on some "wild carrots" he found while he was out working. I Google "wild carrot dosing" and quickly figured out the diagnosis (this was in the this was Northeast USA by the way). I will give you a hint...a certain Greek philosopher also had an affinity for the substance...it was hemlock. AKA: Not good for you.
He recovered fine, though he did get a night in the ICU for observation.
70. Cat Calling
A six-month-old baby was not getting bigger and dropping off the growth charts. The baby wouldn’t move and cried all day long. I couldn’t figure it out. I was making preparations to transfer the baby to the university hospital for admission. One of the clinic nurses commented that the baby's cry sounded like a cat. Ding, a bell went off in my head.
Cri du chat syndrome or cats cry syndrome. Very rare. I looked it up on UpToDate and the baby had a high probability of having it. I referred her to genetics and they confirmed it. The attending called me and marveled at my clinical skills. I chuckled and told him the nurse diagnosed it. Good news, the baby had a small deletion of the 5p chromosome and managed to stay somewhat healthy and functional.
 Pexels
Pexels
71. Hoofbeats
I diagnosed a patient with acute intermittent porphyria. He had a history of psychiatric admissions with depressive symptoms associated with nausea (though not much in the way of pain). I saw him as a medicine consult for the psychiatry service and ordered urine porphyrins just for completeness as it apparently had never been tested before. Lo and behold, they come back positive.
There is this old adage in medical school, "When you hear hoofbeats, think horses not zebras". Which while perhaps relevant to a medical student, is actually the opposite for what is needed from a skilled practitioner. The common stuff is easy...practically reflexive. In our case, a better adage would be, "When you hear hoofbeats don't just assume it’s another horse". Too often physicians just hear the hoofbeats and ignore the black stripes.
 Pexels
Pexels
72. Just a Nibble
When I was on peds ID, we had a young girl come in with a rash on the bottom of her feet. She was also having headaches and joint pains. We spent close to an hour interviewing the girl and her mother. Her history was essentially negative. Finally, as a last-ditch effort, I pulled out the weird questions you ask in med school.
I asked if they had any unusual pets, as we had already ruled out normal pets. They said actually they did just return a pet rat for biting her. They thought that this wasn't really relevant. Bam! Rat bite fever.
73. The Neighbors
An elderly lady came into my practice asking if there was anything she could be given to help her sleep, as the Irish terrorists in the flat below were keeping her awake at night. She was reassured that terrorists were not planning to make her home explode, or Cannock (a small inconsequential town in the West Midlands) for that matter.
On the second visit, she insisted that they were going to detonate whatever they had soon and expressed paranoid thoughts. A full mental health review was conducted by the GP and the community psychiatrist. She came up clean. That's when we contacted the authorities, a couple of days later the flat below our patient was raided and found to be full of explosive equipment and real IRA members.
"How often have I said to you that when you have eliminated the impossible, whatever remains, however improbable, must be the truth"?
 Pexels
Pexels
74. The Line Of Fire
I was in my first year of X-ray school at a community hospital in a mid-sized city. I didn't even know what an enema was before one of the technologists asked me if I wanted to shadow and watch one get done on a 92-year-old lady. I said of course! I watched them help this little white-haired lady get onto the hard table with just a sheet under her.
I then acted super interested so as to look like a star student, but inside I was screaming. What a horrible and disgusting test! I'm so glad I was oblivious to gastrointestinal studies before deciding to go through with X-ray school—I might have decided on another career path. Somehow, though it got worse. No one told me not to stand in the line of fire when we rolled the teeny frail old woman onto her left side...
Let’s just say that I am glad I kept my mouth closed. I was quickly and very quietly guided out of the room, up to the showers, given scrubs to change into, and given the rest of the clinical day off scot-free. My $60 school clinical scrubs were a total loss and put in biohazard trash. I am pretty sure I showered for several hours following getting back to campus.
75. The Solution To All Your Problems
I am the patient, and I am in the middle of this. I don't actually know how it's going to affect me yet. I have always had headaches. In fact, it led me to develop a pain medication addiction, though I’m better now. As anyone with chronic headaches knows, you can always tell when some pain is even a little bit different than normal pain.
One day, I started getting headaches that felt different than usual, so I went to a local doctor. They are free, but most of them are really rushed and don't really care that much. The doctor who I ended up seeing basically said, "I used to be a physiotherapist and I think this is muscle pain. Get some physio and work on your posture". I have worked on my posture for years as a remedy for my ongoing headaches, to the extent that people at work have asked if I was a dancer because I held my spine so erect.
So I didn't think it was that. And you know that saying: “When all you have is a hammer, everything looks like a nail"? I didn't really trust an ex-physio when he immediately said it was physiological without even asking me where the pain was, or what it felt like, or whether it was new. So I got a second opinion.
I later saw an optometrist for my annual check-up. She took one look at my imaging and immediately got me to take some extra tests I hadn't had before. Then, she gave me a referral to an ophthalmologist. She said, "Please go see this doctor as soon as you can".
She looked scared. I said, “What is it”? She said to me, I kid you not, "Have you recently started having headaches on the right side of your head behind the ear"? I replied, “How did you know”? She said, “You have a retinal hemorrhage in your right eye”. Two days later, the ophthalmologist confirmed the hemorrhage. He took more tests.
Eventually, he told me he suspected glaucoma and gave me a referral to get an MRI. I got the MRI a month later and it revealed that I actually have a brain aneurysm. It's small, but it's pressing on my optic nerve and affecting my vision. When I eventually went back to my first doctor, I took GREAT PLEASURE in telling him about the retinal hemorrhage, the increased intraocular pressure, the glaucoma suspect, and the aneurysm.
He just said, "Oh well, I suppose that might be causing headaches". We'll see. I hope if I can get this aneurysm looked at, my new headaches might subside. I am going to see a neurosurgeon soon. Fingers crossed!
76. Show Me Your Teeth
If you have a patient in labor (or in any painful procedure) who wants to hold your hand, only let them hold two fingers. They can't squeeze them too hard and break the bones, yet they still get the comfort of human touch. I've had patients in labor pinch me, pull on my clothes, and squeeze my two fingers as hard as possible. Some are just panicked, but some seem to be angry and want to hurt someone.
I always calmly ask them to stop with the pinching or pulling on my clothes because that really isn't helping them. These are often people who have refused an epidural because they are afraid of needles. While I understand that, I myself refuse to go black and blue. I always teach the new nurses or students the two-finger trick.
Which reminds me: Several years back, I had a couple in for a delivery. I asked what method of pain control they preferred. Their response was bizarre. They looked at each other, giggled, and then he said, "She bites me". I asked for clarification, and apparently, during her first two deliveries when the contraction pain became unbearable, she would take his hand and literally bite the heck out of his knuckle.
They were both hip to this plan and oddly proud of it. Fast forward to a couple of hours—the labor was getting well advanced. I looked up while doing an exam and saw her clamp her teeth on his calloused knuckle. She appeared to be biting with full pressure. He made a bit of a face but not a sound. Soon after, we ushered their youngest into the world.
When the contraction would start, she'd take a lung full of air and push to the count of 10 while biting the heck out of her man. It worked for them, so who am I to judge, but it made me somewhat uncomfortable.
77. An Unholy Terror
I had a 60-year-old female patient show up for a same-day appointment to establish care from out of state. She had no medical records and she denied having any history of taking medications. She never smoked, drank, or anything. Midway through the exam, she started telling me that she was seeing "evil lines" all over her house at all hours of the day.
She said that she was unable to cross the lines and was therefore unable to access certain parts of her house like her bathroom. She claimed to hear voices coming through the walls and feel shadows at night. She also thought her neighbors were hexing her all the time.
At some point, she started talking about the occult and freemasons ruling the world. Then, suddenly, she stopped mid-sentence, stared at me without blinking, and asked if I could perform an exorcism. Err... Sorry. I missed that section in medical school.
78. Face-Palm Parenting
I'm a nurse and I work in a pediatric ER. A young woman brought her baby in to be seen for vomiting. I ask her to put the baby on the scale. While on the scale I notice a strong odor of bug spray so I asked about it. Her response made my blood run cold. Mom: "A roach crawled into her mouth so I sprayed a little Raid in there". She said it in a matter of fact tone, like it was no big deal.
Queue up calls to the authorities, CPS and a 1:1 sitter for the child and the mom. When all was said and done the baby was fine and turned over to her grandmother so no worries there. I have no idea what happened to the mother. I don't believe she was intending to hurt the child. I think she was just completely ignorant.
79. Look Out Below
As a student nurse, I observed a cesarean section when the mother had preeclampsia. The mom was awake with an epidural in place and a screen was in front of her. All went well at first. Her uterus was sewn back up and I was starting to relax...until the surgeon asked the medical student at the foot of the bed to step aside. That's when I witnessed an absolute horror.
The doctor reached in and pumped the uterus twice and hard, forcing the remaining after products out of her fast. The wall wasn’t that far from the foot of the bed, and the student had definitely been in the line of fire. The patient nor the husband didn’t seem to notice, but when the medical student and I looked at each other, she just said, “Whoa”.
80. I Got This
I’ll never forget the comment my labor and delivery nurse made. I had been laboring in the tub at the hospital but wasn’t supposed to actually birth in it. When I suddenly started to feel the baby coming, my husband pulled the emergency cord and the nurses rushed in. Through the haze of baby crowning pain, I heard a panicked nurse say, “I don’t know what to do. What do we do”?
I distinctly remember laughing to myself and I heard my midwife’s calm voice say, “It’s okay, I’ve got it” as she moved past the nurse and took over.
81. A Rare Talent
I've diagnosed anti-NMDA receptor encephalitis in a patient that was thought to be withdrawing from an unknown illicit substance. Then, not two months later I had another patient with the same disease. I was talking to a neurologist recently and he thought it was a condition that is far more common than we thought it was, but still a pretty good catch for an internist.
I've caught a few conditions that were rarer, but it's nice to talk about one that's treatable.
82. The Woman Who Knew Too Much
My twin sister is a nurse. She most definitely didn't learn how to care for her own dying mother in nursing college. Our mother passed from cancer, and we nursed her until the very end at home. I was very thankful that my sister is a nurse and knew what to do, but the minute my mom passed, my sister could not be in the same room.
She had already seen so much tragedy as a nurse before, but nothing could prepare her for her own mother’s passing. I think my sister questioned her choice of being a nurse after that. To me, I was seeing my mom finally being released from all the pain she was feeling. For my sister, she knew what was happening below the surface.
She knew how my mom's lungs were giving in, and that her heart was failing. The thought that she knew that hurt me inside as much as my mom's passing did. I have a lot of love and respect for my sister.
83. Miracle Porridge
I made a clinical diagnosis of fairly early-stage necrotizing fasciitis (the infamous flesh-eating bacteria) in West Africa which was pretty cool... The patient was a young adult male who was writhing and screaming in agony as he was carried in. He spoke a tribal dialect and I spoke ugly French, so it was basically impossible to get any information out of him or the friends who brought him in.
I laid him on the table and did a rapid trauma assessment. When I stripped off his shirt, I saw a small patch (maybe 4" x 6") of blackened tissue below his left nipple along the side of his ribs. It looked like a chemical burn to me at first glance. I realized that some of the skin had torn off the area when I removed his shirt, and when I touched the lesion to examine it, I could feel the skin separating from the tissue below it.
The technical term is "desquamating". It had a horrible odor like spoiled meat/rotting garbage mixed with 100-degree west African heat and 100% humidity. Putrid. His temperature was over 40C (104+ F) and his O2 saturation was terrible. The rotting garbage smell indicated anaerobic bacteria, the skin peeling off indicated connective/soft tissue involvement, and the disproportionate pain (relative to the size of the lesion) is a hallmark of necrotizing fasciitis.
I ran back to my room and grabbed the Oxford Handbook of Tropical Medicine (highly recommend if you work over there in medicine) to double-check because I had never seen a case of flesh-eating bacteria in person before and didn't want to screw up the diagnosis and move things in a different direction if I was wrong. Sure enough, everything matched up and the chief of medicine stopped by to confirm the diagnosis. He basically said, "Oh yeah we see these fairly frequently, people get a cut or a bug bite and then rub dung or dirt into it and the infection takes hold".
The craziest part was the outcome. In the United States, patients with necrotizing fasciitis in one limb frequently die or suffer amputations of both arms and both legs—even in the best ICUs. Here we were in the middle of West Africa at a remote bush hospital and this guy has it on his chest, which pretty much wrecks the standard aggressive surgical approach since you can't exactly amputate the chest.
We loaded him up with high-dose IV ampicillin a few times a day and his wife forced him to eat multiple bowls of porridge...miraculously he made a full recovery and left smiling 10 days later. I'm convinced it was the porridge.
 Unsplash
Unsplash
84. Just A Normal Day At The Office
I never learned how to deal with the unclothed man covered in his own poop who barricaded himself in his room and started commando flinging his mess at anyone who attempted to deescalate him. But I'll tell you this much—I’ve never felt more like Captain America than I have while fully gowned and equipped with a riot shield blocking flung poops coming my way.
85. Torn Apart
My young, newly-married patient got in a bad motorcycle crash with her husband. She survived and her husband didn't. She woke up and started yelling, "Where's my husband"?! Then it got worse. See, we couldn't tell her that he didn't make it, as only the doctor could do that. Unfortunately, the doctor couldn't come up for three hours.
So for three excruciating hours, we couldn't tell her anything. I would walk into her room knowing that her life was about to be destroyed. My gut hurt just thinking about it. I'd ask her, "Can I get you anything, ma'am"? and she'd reply, "I just want to know where my husband is. Is he okay"? I would tell her that I wasn't sure, but no matter how hard I tried to poker face it, I think she could tell in my voice that he was gone. There's no chapter on that in any textbook.
86. The Meat of the Issue
A patient came in with an itchy rash that would not go away for weeks, and a new swelling of the mouth and tongue. She had "hives" all over her body and the only thing that had helped was repeated steroids. She was a mid 40s female who worked with dogs, so we assumed that she had a new allergy to pet dandruff, fragrance in a shampoo, flea medicine, or something along those lines. We discharged her home with an appointment for the dermatologist to do a biopsy of the lesions. But that wasn't the last we'd see of her.
Later that day, she turns back up in the Emergency Department with swollen lips, increased rash, and trouble breathing. She started having these problems 15 minutes after eating a roast beef sandwich. Someone on the team remembered that she works with dogs and asked if she'd had any recent tick bites. Sure enough, she had been bitten by a tick a few weeks ago and identified a picture of a Lone Star Tick.
Turns out she had developed an allergy to red meat after a bite from that tick. This allergy is called an alpha-galactosidase allergy, and is a reaction to a carbohydrate carried on the outside of cells (think like the carbohydrates on red blood cells for ABO blood type) by all other mammals except humans and monkeys.
The tick had bitten one of these and kept some of the protein in its digestive system, and then after biting her, her body developed antibodies to the carbohydrate, causing her to have a new allergy to meat.
87. A Leg Up
We had a patient who was homeless and taken to our ER. During that time, we found out that he had stage 4 metastatic cancer with only a few weeks or months left to live. Our unit was a short-term stay unit, so we kept the guy. At the time, he had been off his anti-psychotic medications and we needed to restart them. But…it was a tough transition.
For a short time, we had to take away his prosthetic leg because he would throw it at anyone who walked in the room. We, of course, made sure he got up and around with a wheelchair, but never in school did they tell me a prosthetic leg may be used against you.
88. Non-FDA Methods
We had a case a couple of years ago that still gives me chills whenever I think about it. A younger girl goes to her family doctor in a small town outside of the bigger city where I live. She had persistent headaches, which just started a few days prior. No past medical history of anything similar or really at all about her that stood out as relevant.
Unable to diagnose or treat her headaches (which were rapidly growing more severe), she was sent to our hospital (X state's Childrens' Hospital) for evaluation. We ran her through the typical gauntlet of testing for common causes, CBC/CMB/CT/MRI, etc. still with no clue. Nothing came up on blood cultures either. At this point, she was in the PICU rapidly deteriorating, with high fevers and periodic losses of consciousness.
After eliminating all the horses, we had to start looking for zebras...and quick. We collected a CSF sample for culture thinking it might be one of the rarer forms of bacterial meningitis. While this was cooking (cultures usually take at least a few days) we tried again to get any other possible info from her parents...that's when we learned the whole story.
For the first time, they mentioned that they had visited a local waterpark a week or two before the girl’s symptoms started...and this was in the middle of summer. For any Peds doctor, or especially ID doctors in the room, those words made their hearts sink. Sure enough, the cultures came back, positive for Naegleria Fowleri, the pathogen responsible for Primary Amoebic Meningoencephalitis (PAM). Which up until that point, I don't think there was a documented case of a patient being diagnosed with PAM who survived.
It’s the incurable brain-eating amoeba that lives in warm stagnant water and can enter through the cribriform plate at the top of the nose if the patient gets water up there...which happens all the time at waterparks. Anyway, long story short, we basically cook up a (very non-FDA-approved) drug cocktail as a sort of Hail-Mary attempt at fighting this infection, as nothing else in any other case had ever worked.
In addition to this, we basically stick her in a Mr. Freeze chamber, lowering her body temp to below what N. Fowleri can usually survive. Unfortunately, most people can't survive it either. But for some reason, (though in an induced coma the whole time) she steadily improved. When we took her out of the deep freeze and allowed her to wake up, it was incredible...
She was alive with no apparent neuro/cognitive deficits, and the new cultures showed no growth of N. Fowleri. It's not too hard to figure out where this occurred, as it may still be the only successfully treated case in the US.
 Unsplash
Unsplash
89. Jaw-Dropping News
I'm not sure if I count because I'm a veterinarian, but I saw trigeminal neuritis in a dog. Basically, the dog can't move his lower jaw, but it's not stiff or painful or anything, it just hangs slightly open. It looks like the dog has just received some unbelievable news, basically. It goes away on its own in 2-4 weeks, but the dog can't eat or drink very well, so you have to syringe feed them, do elevated food bowls, etc.
 Needpix
Needpix
90. Improvise. Adapt. Overcome.
I'm PhD, not MD. The weirdest to me was a bloodstream bacterial infection that looked sensitive to antibiotics in the clinical lab, but the patient could not be cured. We got samples of the bacteria and turns out it was "tolerant" to antibiotics in a biofilm (heart valves) but not sensitive in the clinical sense. Opened my mind as a microbiologist to how insanely adaptive bacteria can be, and how they're more a population than individual cells. The most interesting paper I ever published, and unexpected.
91. Cruel To Be Kind
Before practicing, I use to think death was the worst possible outcome. After working in the ICU for 10 years, I feel as though the staff is sometimes forced to prolong life despite the morality of it. I would even go as far as to say we put patients through long, arduous torment and suffering. For example, I took care of this patient in a neurosurgical ICU that had a massive brain aneurysm that ruptured.
He came to the hospital and went straight to the operating room to remove large parts of the skull to allow for his brain swelling. Weeks went by and the patient never recovered. The patient only had some minimal reflexes. He was basically unresponsive—he couldn't move any of his extremities. However, the patient was not clinically braindead.
Despite many meetings between the healthcare staff and the family about the severity of the injury and the 0% chance of the patient having a meaningful recovery, the family decided that they wanted us to do all that we could to sustain his life. It all went wrong in the worst ways. Over three months of being in the ICU, the patient developed huge bed sores from not being able to be turned due to his critical injuries.
He also developed necrotic appendages in his feet, ears, hands, and nose as well as worsening swelling of the brain. It became so prominent that the patient's head incisions started to split open. Eventually, multi-organ failure set in and he ended up passing via a slow, painful end. Such a horrible situation, and one that I regret to this day.
92. Benadryl To The Rescue
I had a patient transferred to our hospital for a STEMI (major heart attack). When they arrived, I noticed they looked a bit red and asked them, other than the chest pain, what symptoms they were having. The person said that they had been having a rash for a few days as well as nausea, vomiting, and diarrhea. Those symptoms go along with a condition called scombroid poisoning which you get from eating old, dark meat fish (tuna, mackerel, etc.).
I asked the person if they had recently been eating fish and sure enough, they had been eating salmon for the past few days. Assuming they had it, I treated them with Benadryl which fixed the rash, nausea, vomiting, and diarrhea. They were taken by the cardiology service to get a cardiac catheterization (how you find clogged blood vessels in the heart) for the heart attack and the results came back normal (no vessel occlusion).
Best I could tell, the condition stressed their body and made them tachycardic/hypotensive which made their heart work harder. The increased demand on the heart + an already weak heart led to the heart attack. Also, was pretty awesome to see the EKG go from showing a clear heart attack to normal after being treated with Benadryl!
93. Agnes Gets Her Groove Back
People with dementia sometimes forget some or all of their own family members. They also forget common social decorum. By the time the patients are with us, the family realizes that the end is near, so a lot of people that weren’t always present in the patient’s life start showing up.
After the shock disappears, the family then begins to see their relative as just any other person. The grandpa, grandma, mom, dad, whatever, ceases to exist. The patient kind of becomes their true unfiltered self in a way. Some families get the bittersweet fortune of getting to see this person how their friends might see them. Not that this is always good…
At some point, it almost always turns into the patient getting rather, uh “intimate” in their conversations. Sometimes, they even hit on a younger attractive family member. People usually take it in stride and understand the situation. But there are times when the patients lose it when they find out grandma “wants a ride on him”.
94. Subtle Symptoms
Not super rare but sort of diagnosed/missed Myasthenia gravis. I was an intern in the emergency department. A woman presents with the classic vague symptoms of fatigue and weakness. Notably, her father had very recently passed. The full blood panel was normal, her examination was almost completely normal but I did find she had a proximal weakness (her upper arm strength and thigh strength were poor but her hand and feet and shins, etc. were normal).
I presented to my superior and we decided to send her home because we couldn't diagnose her with anything and we can't admit someone to the hospital for fatigue. She was upset that we couldn't help her. After she left, I couldn't shake this terrible feeling. I asked my superior, what about Myasthenia Gravis? Well, too late now, besides the testing takes weeks.
She represented a week later (I didn’t see her). She was admitted this time and seen by a physician. More tests were ordered and eventually, she was diagnosed and treated for Myasthenia Gravis. I saw her 6 months later and she remembered me, she was doing much better and wasn't upset that we missed the diagnosis.
It can be very hard to diagnose some things because of how non-specific the symptoms are. In this case, I had a feeling she had a real disease especially with her proximal weakness but there wasn't much we could do about it.
95. The Rear View
Nurse here. A very panicked nursing assistant came running to the desk one day, saying, “You have to see this! I don’t know what this is”! She then brought me into a private room where she was giving the patient a bath. She pointed to an area on the patient’s buttocks. “What is that”? I leaned in for a closer inspection, and my face went white.
The patient then started to turn back around and said, “IS THAT MY EYE”?! Sure enough, my patient had a prosthetic eye that came out of the socket at some point and it became suction-cupped to her buttock. I left the room and had never laughed so hard in my life. Truly one of the most bizarre and hilarious moments in my career.
96. A Bad Bridge to Cross
In dental school, I had an emergency patient come in complaining of sore gums. Upon examination, I found a massive calculus bridge (google it for pictures) behind her lower front teeth. She only had about 3 remaining lower teeth, but they were all connected with a whitish brown mineral deposit that was about the size of a golf ball. She had never had her teeth cleaned and she was probably 55 years old or so.
I basically performed an emergency cleaning. She could speak so much better afterward. Of course, I had to play it off like it was normal, but in my years of practice, I still haven’t seen a case that bad again. Get your teeth cleaned people. Even if you can’t afford every 6 months, once a year, or every other year is a heck of a lot better than never.
 Pexels
Pexels
97. Fancy Seeing You Here
One of my patients was having pain whenever she peed. I did a standard UTI and STI panel, particularly for chlamydia. It was a self-test, so I had to explain to him the basic procedure of inserting the swab and twirling. The poor guy was so uncomfortable—not that I blame him—but my hardest task was explaining it all with a straight face. He had come from work so he was still in “uniform”. He was a priest.
98. Like Flipping A Switch
I can't remember all the details though so bear with me. I'm at a big tertiary hospital and had an elderly veteran brought to us one day after being found unconscious in a park. He had alcohol in his system and a quick look at his records showed that this was an ongoing problem with him. He was a sweet old man who was very grateful for our help, up until day 3 of his hospitalization. That's when things took a dark turn.
He developed pneumonia-like symptoms and became somnolent for a few days. Then, out of nowhere, he became very inappropriate—he begins grabbing the nurses and repositioning them, touching himself, and constantly licking his lips in a disgusting manner when anyone even looked at him. He went from a sweet old man to a deviant almost overnight. We even had to wrap his hands up in bandages to stop him from touching himself and others. Oddly though, he hit on anyone and everyone (women and men) except for me. I guess I wasn't his type.
We ended up diagnosing him with Kluver-Bucy syndrome, caused by HSV encephalitis (herpes). Symptoms include hypersexuality and hyperorality. It's pretty rare and I haven't seen it since, but as you might imagine, it left a lasting impression on me. He improved with treatment though and was incredibly embarrassed after finding out what he had done.
 Pexels
Pexels
99. A Tickle Under The Rib
I saw this one patient with a really odd condition. While she was asking me why she gets rib pain so often, she literally reached under her own rib and jiggled it with her fingers. Turns out, there were a lot of other things she could do that she shouldn’t ever be able to. I attributed it to a variant of Ehlers Danlos syndrome, which causes connective tissue abnormalities.
I was so distracted by the popping in and out of her rib that initially, I didn’t even notice how horrifying it was that she could get her hand under there.
100. Well, I Guess That’s One Way to Travel...
First physical of my life. I drop my pants and the doctor says turn your head and cough. For some odd reason that I cannot quite understand, I thought he said turn your head and crawl. I cannot explain the levels of confusion and awkwardness that followed when I started to nonchalantly crawl around on the floor of his office…
101. Lifesaver
I work as an ER nurse and had a patient with a little dizziness, a little nausea and a swollen abdomen. She was fairly bright, able to talk, and nothing seemed too horrific. But she was turning a grim gray color and breathing quickly. Our average wait time today was two hours. I could have put her back in the queue and moved on.
But I had a little dark feeling that there was something sinister happening here. So I called our most senior doctor out of a consultation and asked him to see her. Right now. Ever heard of your abdominal aorta? Enormous blood vessel that can pouch out, suddenly rupture, and make you bleed internally until you perish in minutes?
It’s called a burst AAA (abdominal aortic aneurysm). You’ve heard of it now. That’s what she had. I’ve never seen one before. But now I have. Within five minutes, she was barely responding. Within ten, her blood pressure had dropped to a barely sustainable level. Within twenty minutes, I was pouring blood into her and eight people were around the bed.
Within an hour, she was on an operating table clinging to life. But because I raised the alarm, and because my team worked their butts off, that woman is still, somehow, alive. Feels good, man.
102. A Real-Life Zombie
I had a lady come into the ER listed as having “Multiple Medical Problems”. This usually means diabetes and the issues stemming from it, or maybe bleeding issues from another disease or maybe odd blood tests results at a clinic. I hadn’t seen the patient yet, but the doctor came to the nurse’s station asking who had room 15. I jumped up and followed him into the room.
I walked in and saw what I thought was a body. Then the patient’s eye swiveled over to look at me. She truly looked like one of the people they found in a concentration camp. I could see every bone, and her body was twisted in a decorticate position with her jaw locked open. Then the smell hit me: rotting flesh and body fluids. I struggled to keep a neutral face and not gag.
I tried to place a blood pressure cuff on her arm and her skin just started flaking off in my hands. I gagged. The doctor started removing her clothes to examine her. Her feet were black to the ankles. Her hip bones were poking through her skin and were black. The skin around her ribs was worn away to oozing muscle fibers.
Her calves were incredibly swollen and the skin was splitting like ripped pants. I removed her Depends, and there was excrement coating her entire genital area. Then the doctor went to remove a large bandage on her lower back. Her entire sacrum was exposed and the bones were BLACK! The skin around it was a black liquified mass.
It smelled like nothing I’ve ever smelled. I can’t even describe it. The doctor told her family I would clean up her ulcers and wounds in preparation for surgery (liar, no surgeon would operate on her). I had no idea how to clean dead bone tissue and liquified skin (they don’t cover that in nursing school). When I went to clean her sacral area, all the liquified skin separated and oozed all over the bed. I really struggled to keep myself together.
Afterward, I needed a moment in the supply closet to cry it out for a second. I had no idea the human body could break down so much without dying. I still think about that woman sometimes, and what led to her living like that. It still breaks my heart. My guess is that she had some sort of traumatic brain issue or a stroke.
Family members were taking care of her, and I think they were treating her absolutely horribly. I think as her skin deteriorated, she developed terrible pressure ulcers that never healed. The swelling was probably due to starvation and a lack of protein in her diet. I’ve had nightmares about her face since then. Once, I dreamed she crawled into bed with me.
I freaked the heck out and ran into the hallway. My toddler walked out after me, rubbing his eyes, asking why I ran away.