Every day on the job, doctors and other medical professionals make split-second decisions, sometimes based only on a feeling. These Quora users tell the most dramatic times those gut feelings turned out to be true.
1. The Long Goodbye
It was Saturday morning, and I had just endured 2 days of OR chaos with an arrogant, narcissistic surgeon, who was, yes, “all that” and more. I was mentally and physically exhausted, and only wanted to stay at home with my kids and make pancakes.
But, the call came at 9:30. I was working the cardiac OR call shift, and it was an “on-call” for an emergency return-to-surgery patient. It was a terribly congested stormy Saturday morning drive to get to the hospital, traffic was slow, and I was beyond the expected 30-minute arrival time.
The surgeon was more than angry and doing his best to rush everyone into the OR. More was to come. The patient, I discovered, was the survivor of a horrible operation that had taken 28 hours—I had been in that surgery too, just didn’t know he was the patient. The patient, Rob, was a young man, early thirties, with a congenital heart valve defect.
The previous surgery, on Thursday, had been to replace the valve. Rob had had several heart/health issues. His mother was his ultimate strength and support throughout his life. It had been a sudden decision that day to return to surgery due to declining status, so I understood WHY the surgeon was in a hurry.
Also, it was the same surgeon who had “performed” (I’d say; “messed up”) the first surgery. Rob’s family lived further away than me and, with the heavy traffic, had not yet seen or talked to their son. He was anxious. I saw that he really needed something more.
The practice was for the circulating nurse to do the final patient interview just prior to entering the OR, right outside the double doors. This is where the nurse ensures that this is the correct patient for the correct procedure, correct side, site marked, consent signed, allergies checked. We did all that.
I knew Rob from Thursday, and he remembered me. After the required questions/answers, Rob hesitated, and gripped my hand. His words nearly broke me. “Do you have a son?” he asked. “Why yes,” I smiled. “I have two sons”. I could see his deep brown eyes, and he could see my intent green eyes.
“Did you hug them this morning?” “Of course I did”. I paused. I remembered Rob’s family. I knew that they were NOT there, today. “Would you like a hug?” And he nodded. He whispered how much he loved how his mom would hug him and stroke his hair (I did).
He told me the song she sang (I did). He joined in, in a croaking, yet moving voice. A new resident poked his head out of the OR and told me if that patient was not in the room in 3 seconds the doc was going to “write me up”. But I had an instant comeback. I respectfully told the resident to give him a pen. And paper, if he needed it.
The new resident gulped and withdrew. The OR doors shook with the vehemence inside. All this had taken 2 minutes by the clock. Rob told me his favorite prayer. We said it. He told me to remember to hug my sons every day. I promised I would. He asked if the sun was shining today and I told him about the miserable rainstorm that was holding up traffic.
“Well, there’s my answer. Mom and Dad aren’t supposed to be here. We can go in now”. Then I knew. Once again, I stopped the anesthesia resident from moving the gurney forward. I looked into Rob’s unfathomable eyes. Took a deep breath, and a leap of faith.
“What shall I tell your mom?” I asked. He nodded, gave me a smile. His eyes now sparkled, and peace enveloped his former trepidation. “That she is the best mom ever. And I’ll wait for her”.
I let Rob see the tears in my eyes. “I’ll find a way” I managed to speak without the waver my soul felt. Then I gave him a thumbs-up.
We went into the OR and the surgeon let out a string of invective before the patient was even transferred to the OR table. I gave him the “look” that my residents and children feared. This surgeon pretended not to notice. I held Rob’s hand as anesthesia was induced.
He worried that I was in trouble. “Nope!” I assured him. “You just think of your mom now. I’ve got you”. We held eye contact until he was peacefully “sleeping”. Four-and-a-half grueling hours later, Robe passed on the OR table.
The surgeon blamed me for taking so long outside the doors. He burst out of the room, in complete rage, to talk to the family. Twenty minutes later, I did something very unusual. I went to the family room. It was not in my job description, nor expected, nor the norm.
I was uncertain to step out of my professional boundaries. But, Rob and I had history. Mom, Dad, and brother were there, quietly grieving, quietly blaming themselves for “not being there”. This was not right.
Quietly, I asked permission to talk with them. I told them that I was the nurse who took Rob to surgery, today, and on Thursday. Would they like to know what he said? It was like I gave them the moon. I told them how we talked about sons, and hugs, and how much Rob had loved his mother’s hugs and how I’d stroked his hair, as he had described how his mom did for him when he was worried.
I told them about Rob’s favorite song, and how great he was with those low notes. I recited the prayer. And then I told Mom that Rob had a message for her: How much he loved and appreciated her, and that he would wait for her. And, I hoped they didn’t mind, but I hugged Rob for them.
The family was overwhelmed, tearful, happy, sad, incoherent, and in a jumbled-up fashion revealed that I had given them the next best thing to saying “goodbye” to their son. They told me they weren’t sure if they could have handled that at all—and the traffic snarls enhanced their fears.
“What does a parent say to a son, when you want to give hope but both sides just know there is none?” So Rob was right. I was right. The surgeon was angry and wrote me up. But there was a twist. The family wrote such letters of commendation for me that I didn’t get into trouble. The surgeon, however, did.
That surgeon was not allowed to operate without senior staff to supervise for a long time. I worked in the OR for many years, and always taught new staff members to NEVER hurry a patient into the OR if they have something to say. It could be the last thing they say, and will be a priceless gift for a grieving family. Everyone is important.
2. It Comes Without A Warning
I get gut feelings quite a lot. Sometimes a patient‘s vitals are reading perfectly normal. We have something called the National Early Warning Score that charts a patient’s vital signs and calculates a numerical value. But even if a patient looks “medically well,” there’s sometimes a much bigger picture at play.
So then we do something called an A-E assessment. If I’m not happy with a patient’s condition, then my job is to escalate it to a medic regardless of their NEWS score. Sometimes a gut feeling is the difference between life and not.
3. Don’t Judge A Tumor By Its Cover
I was administering the anesthesia for a neurosurgeon friend. He was removing a cervical spinal cord tumor of a woman in her late 40s. She was prone (on her stomach) on the table. He is an excellent surgeon and fun to watch work, no extraneous motions.
I had just turned my back to the field and was doing a routine check of endotracheal tube placement to make sure it had not migrated. With the tumor now completely exposed, he asked for the scalpel. Then I saw it. With my back still turned, I quickly called out “Stop!”
Everyone turned and looked at me. He asked me why. I looked at the tumor one more time and asked him if he would mind aspirating the tumor, because something about seemed funky to me, even though I had no evidence. He said all of the X-Ray reports had confirmed it was a solid mass tumor. But, because of our long history, he said he would humor me.
The nurse gave him the syringe. He pulled back on the plunger and blood returned. Only he and I realized what had just happened. Later, he explained to the nurses that there would have been almost no way to have stopped the bleeding if he had made the incision without aspirating, and we may have very well lost the patient.
4. A Rush Job
I'm not a doctor or a nurse. I was just an ER admit clerk. There's supposed to be a triage nurse on duty at all times but once in a while it happens that the nurse isn't on station. Once a young Hmong couple came up to the window where I was working.
The woman carried a small baby in a blanket. I looked up at them and immediately knew something was wrong. I jumped up from my desk, opened the door, and took the wrapped-up child in my arms. I motioned to the couple to follow me, and I almost ran to the back.
I found the charge nurse and handed the child over. I had not even looked at the bunched-up baby but I said, “Something is wrong”. I stepped back and the nurse opened the blankets around a little tiny child and saw a blue baby.
Immediately the charge nurse went into action and quickly the child was placed on oxygen and other services were provided. The Hmong couple did not speak English and no one at the hospital spoke the Hmong language at that time, but the child was saved because they came in quickly and, I was told later, because I grabbed the child and took it immediately to the back instead of calling for a triage nurse to come to the front.
5. Not His Chipper Self
There was a patient I had who was feisty and sort of smart-alecky, as they say. He was a retired veteran from the US Navy. I had him as my patient for two days, but had a day break from him and was now back with him as my patient.
Usually when I went in to greet him, he would have a feisty greeting for me—but not that morning. I tried to engage him in conversation, but he wasn’t returning the banter as he usually did. Something wasn’t sitting okay with me.
I paged for my medic, who took my patient’s vitals. He read them to me and they were all within normal findings. But still, my patient was not acting normal. I decided to make a phone call to my intern team for the limb preservation team.
The intern said, “Vitals are normal and when I am done making rounds, I will come up there”. I still could not shake the feeling something was wrong with my normally salty, feisty patient. I still to this day remember his name and what he looked like.
I called the intern back and said, “Look, I don’t have any abnormal vitals but if you come and look at him you will see he isn’t the same. He is usually feisty and salty in demeanor and today he isn’t engaging in talk”. The intern said again he would be up when rounds were finished, which would be in about two hours.
I decided to call the staff doctor of the limb preservation team, Dr. Andersen. He listened to me and said, “No problem, I will be right up there”. I explained, “I have the vitals taken again and they are normal, but he is just not himself. I know this patient well and something is off”.
Dr. Andersen said, “Don’t worry. It’s all okay. I trust your instincts”. When he got up to my unit, he called the interns and told them, “When the nurses on the units call you to come up and they know something is off, you listen to them”. It ended up being that he was dehydrated and he had an infection starting at his pacemaker implantation site, all of which was not showing up on his vitals or labs.
So my gut instinct was correct and I’m thankful the staff was willing to listen to me as a nurse.
6. Not Quite Right
I was working in our high dependency bay with 2 of us to 4 patients. I’d been chatting to a lady all day and we’d been laughing and joking with each other. I go to give her a bed bath and notice her abdomen is swollen, which isn’t that unusual after a radical hysterectomy. But it got worse. I was talking to her and some of her answers seemed strange, too.
So, after I’d finished I did a set of observations on her. They were fine but my spidey-senses were still tingling. I informed the nurse in charge of the bay, who said that if her vitals were fine there was nothing to worry about. I went back in to talk to her and she started telling me about dating Elvis…
Now I know something serious is wrong. I go back to the head nurse, who told me to stop wasting her time. I informed her that I believed something serious was wrong and would be documenting in the notes that I had tried to get her assistance twice and was dismissed both times.
At this, the nurse sighed and said she’d go and take a look. The ward sister who had observed all of this just looked up at me from her notes and said “clever girl”. The upshot was that she was in kidney failure and had over 2 liters of urine in her bladder.
I just happened to have been there at the start when her observations were still within the tolerable limits. If you have a feeling something is wrong, always act on it. I would rather look like a fool than have something happen to a patient that could be avoided.
7. Straight Through The Heart
Every good nurse gets a 6th sense about things. For example, one day while I was triaging a patient, a young man arrived to registration. He told the clerk he had been hit in the chest by a BB. I immediately got up and went to check him.
He had a very small, blackened mark just left of his sternum. It looked like a little burned area. It did not look like the BB penetrated the skin. BUT his lips were just a little pale. He said he was scared because his mom was going to be mad that he and his friend played with the BB.
I just got a funny feeling that I needed to have him immediately checked, so I brought him to the trauma room and called a Trauma Team. The arriving doctors were upset and asked why I called a trauma on such a minor injury. I said I just had a feeling it was something that needed immediate attention.
They verbally chastised me, but I said I would not back down. It was my call as the triaging nurse to require them to assess him as a trauma. I was also the charge nurse and went back out to the department. 10 minutes later, I got my answer. The trauma surgeon came flying out of the trauma room and asked me again what made me call a trauma.
I again said it was that his lips looked a little pale, and the spot on his chest was close to where his heart was underneath. The surgeon grabbed my hand and said…“You are amazing! You saved this boy’s life. We are rushing him to surgery. The BB did penetrate his chest and is in the pericardial sack. He is bleeding and needs STAT surgery”.
8. Deliverance
I'm a midwife. I once had a pregnant patient call me about some upper abdominal pain. She was about 35 weeks pregnant. She had no other prenatal problems, just a sharp pain in her upper abdomen. No contractions, normal pregnancy so far.
It sounded like gas pain over the phone. I advised her to have her husband run out to the store for some gas-ex and try that, and some hot tea. I RARELY call people back, but her story nagged at me for some reason. About 3 hours later, I called her again to see if she felt any better, which she did not.
Moreover, the husband still hadn't gone to the store. I asked her to press hard on the painful spot to see if it hurt worse when doing so, and it did not. So I told her to come into labor and delivery to be checked out.
Although her blood pressure was ok, her lab work was AWFUL. She was on death’s door. Her platelet count was 5,000. Delivery is the only treatment, and she spent the next week in the ICU. She did send me the nicest card thanking me for saving her life. Now that's an example of having that weird sixth sense feeling.
9. What A Headache
I'm not a nurse, but my mom was an Emergency room RN for many years. Back during the Sydney Olympic games she was working as a volunteer at one of the medical tents. One afternoon, this young woman walked into the tent and asked if they had anything for a migraine.
Apparently, she suffered from them from time to time, but my mom just had a “feeling”. So she gave the woman a hot drink and showed her to a fold-out bed where she could “lie down for a bit”. She then quickly turned to the trainee nurses on duty and whispered, out of earshot, “It's not a migraine. She's having a stroke. Call 000!”
Which they did and the young woman was rushed to hospital. A few hours later, my mom received a call from the woman, thanking her. It turned out she was right. Despite not showing the classic signs of a stroke, that was indeed what was happening.
Thanks to my mom’s gut feeling, she made it to the hospital with enough time for the damage to be reversed.
10. VIP Patient
An elderly man was led into the emergency room through the back door by his family. People came in the wrong door from time to time and one of the staff was directing them towards the front, but I took one look at the man and I knew he was gravely ill.
I stepped in and took him to a bed and directed the family to continue up front to sign him in. I turned to the paramedic, “Get Debra” (the doctor), to the clerk, “Call respiratory, EKG, notify CT we have a triple A”. All while I am lying him down.
His complaint is back pain. His complexion is grey. I don’t know why I took one look at him and knew that he had a dissection abdominal aortic aneurysm, but he did. He was in surgery within 30 minutes. Three months later, the same doctor called me to come to the waiting room.
I went and that same man is there with his whole family. He was pink this time. There are flowers and balloons, and he is there to thank the doctor for saving his life. The doctor called me over and introduced me to the man and told him that I saved his life.
I usually had a feeling if a patient was going bad. I think a lot of nurses have spidey senses.
11. It’s Not What You Think It Is
One day, a patient came to my practice. She had been suffering from headaches for one week, a pain she had never had before. These headaches were not terrible, they were just unusual; she explained the pain was at the top of her head. It was also constant and not influenced by medicine.
I gave her a muscle relaxant because I thought she might have tension headaches. She had no neurological involvement, no other symptoms. I thought the pain might just subside by the end of the following week. I was very wrong. Several days later she came back and when I asked her to bend over, she said the pain was throbbing in her forehead.
Then I thought she might have sinusitis, since she was working in a place with a lot of cold air and open doors (we were in winter) but it didn’t really seem correct to me. I just hadn’t any clue as how to define this kind of pain. I gave her an antibiotic for three days and asked her to come back three days later.
When she came back, no improvement! She said maybe she would like to have a course of physical therapy since she had a lot of stress, and maybe it was the muscles all the same.
But then this strange feeling urged me to send her for an MRI. It was programmed two days later.
That day, right after she had had the MRI (10 days after her first complaint) I received an email from the radiology institute. The message made me gasp. She had a glioblastoma. I couldn’t believe what I was reading. Glioblastoma. One of the most aggressive brain tumors.
She had such a life of pain, deceptions, and deaths in her family. She was just hoping to retire one day, see her daughter marry, and have kids. I couldn’t believe I had to announce it to her. We called her immediately and she came with her partner.
I didn’t dare to say what it was exactly, for me it’s necessary to have the results of the biopsy before you can say something about survival. Three days later she was seeing a neurosurgeon and the same week, she was operated. This was last week.
For a malignant brain tumor, she is now doing remarkably well. I still haven’t got the results of the biopsy although the neurosurgeon confirmed the diagnosis based on the MRI (a typical appearance).
Although this brain tumor may seem rare, it’s unfortunately frequent. Considering its severity and sometimes poor prognosis, I think it’s absolutely necessary to further investigate any headache that doesn’t fall right away into a precise category in order to rule this diagnosis out.
A quick and correct diagnosis allows these patients to be alive and without any residual symptoms, sometimes, 10 years after the diagnosis. The almost complete resection of this tumor, combined with adjuvant therapies, can allow, in some cases, a very long and symptom-free survival.
12. It’s All Going Wrong
This happened when I was a nurse practitioner student doing a clinical rotation at a busy Urgent Care. A female patient came in looking like the Grim Reaper warmed over. It was obvious she was very sick—fever, increased heart rate, weak, nausea, etc.
However, her symptoms did not fit an obvious cause like the flu. After obtaining a history and performing a physical exam, I went to get my preceptor and told her that I had a real bad feeling about this patient. I’ll never forget, my preceptor, an awesome nurse practitioner with 40 years’ experience, said, “Always trust your gut”.
She came in to look at the patient and agreed something was seriously wrong, but she also couldn’t figure out what. The patient said she needed to pee, so we asked her to go ahead and give us a urine sample. I couldn’t believe my eyes. When the patient returned with the urine sample, it was brown (tea-colored). Red alert!
Tea-colored or red urine is always extremely serious. We called 9-1-1. The Urgent Care was part of a large hospital system, so we were able to track the patient’s progress. Turned out she had Legionnaire’s Disease, kidney failure, and sepsis, along with some other issues.
If she had waited even one more day to seek care, she would have been a goner. She came close as it was, but fortunately made a full recovery.
13. A Stopped Clock Is Right Twice A Day
A female patient came in who was a bit of a hypochondriac. She had seen another provider who kind of dismissed her complaints. A couple days later, she came to see me, complaining of feeling sick and just a bad feeling that something was wrong and it was getting worse.
She looked quite ill. I took history and did a physical exam. There was nothing obvious, but I could tell something was wrong and again, I had a bad gut feeling. I asked her to leave a urine sample. While she was in the bathroom, her husband asked me if he should take her to the ER.
I had been thinking the same thing. He said he knew she was a hypochondriac, but he had a bad feeling. So, I told him he knew his wife better than anyone else and if he had a bad feeling, he should trust that. I told him I also shared his concern and if it were my spouse, I would take them to the ER.
So he did. I called the patient the next day to check on her and she had been admitted to the hospital. Turned out she had an abscess at the back of her throat and had developed sepsis. It took the hospital 3 days to figure this out.
It’s a good hospital, but it just wasn’t obvious what was wrong. She was in the hospital for 2 weeks and made a full recovery.
14. Too Little, Too Late
Yes. And she was gone 24 hours later. I was caring for an elderly woman who had taken a few spills at her assisted living home that resulted in a fracture. She came to us for rehabilitation with the plan of being discharged back to assisted living.
Her stay was only expected to be 3–4 weeks. She was very hard of hearing but one of the sweetest ladies I ever had the pleasure of caring for. Her family was equally as kind. During her third week with us, she developed a cough.
The cough quickly turned into general malaise with an added low-grade fever, and her lung sounds were junky. She was so tired, started having setbacks in therapy, and was sleeping a lot. This was Wednesday, my “Monday,” and my spidey-senses were tingling.
I was suspecting early sepsis, based solely off the mild fever and how she “looked”. I had a gut for sepsis. I contacted our supervisor early in the shift and let her know I was concerned. She disagreed with my sepsis theory and suggested possible pneumonia, so off to outpatient X-ray it was.
I arranged the appointment and transport, all while thinking pneumonia could lead to sepsis but at least an X-ray will show something. Her daughter was in town and accompanied her to the appointment, but she had to catch a flight later that afternoon so I knew it would be a quick turnaround.
When they returned to the facility, I could tell my resident was exhausted. The appointment had taken everything she had. My wonderful aides got her comfortable in bed, and I had a chat with the daughter about how the X-ray had gone, and shortly after she headed for the airport.
I remember standing at the med cart talking to her as she teared up, telling me how guilty she felt for having to leave. I touched her hand and smiled softly as I told her that her mother was in good hands and it was going to be okay. It was not going to be okay. I told her to fly home and see her family and to call me when she got there.
I’ll never forget that conversation. My resident showed no real change through the rest of my shift. No improvements but no worsening either. Wednesday night. Thursday morning. The second day in my three-day rotation. 6:30 am. I came in and received report.
My sweet lady friend had experienced some drops in her oxygen saturation—a sign for both pneumonia and for sepsis, go figure—and the night nurse had put her on some supplemental oxygen. Otherwise, the night was uneventful.
My CNAs obtained morning vitals and all seemed within normal limits, and I got started on my morning med pass. I talked to the supervisor and gave her an update. No imaging results yet. Breakfast comes and my aides pass out trays and get folks set up to eat their meals.
This resident had a neighbor in a semi-private room who had a very strict preference on when she wanted her meds. 9:00 and not a moment sooner or later. You’d hear about it. And that day I was late. I talked her off the ledge, got a smile as she took her pills, and stepped out into the shared entrance.
I peeked over into my resident's room and could see her sitting upright in bed with her breakfast in front of her, working on oatmeal and coffee. “She looks miserable,” I thought to myself. She would be next on my list for meds.
She only took a few pills, which was impressive for someone of her age, so she was a quick pull. It was probably no more than 10 minutes between leaving her roommate and re-entering her room. I stopped at the doorway like usual, knocked loudly, and said “Good morning!”
No response. My stomach dropped. I knocked again, harder, and said “Good morning” again. Louder. No response. And I knew. I walked over to her bed, touched her shoulder, and gently shook it. I said her name. But I knew.
I set her pills down and checked for a pulse. When I felt none, I started my pronouncing assessment. No heart tones. No lung sounds. Pupils fixed. Coffee cup in hand. I tried for two hours to get a hold of her adult children. One by one they all called me back. And one by one I had to tell them their mother had very unexpectedly and very peacefully passed.
The last one was the daughter I’d comforted the day before. I’ve made those calls before, and since, but none like that one. When I sent out a facility notification of her expiration, the supervisor called me and said, “What happened?!” Later that day she said, “I guess you were right”.
I’d never wanted to not be told I was right so badly in my nursing career. I cried the whole way home and didn’t eat for a day after that. It tore me up for a couple of weeks.
15. Going To Great Lengths
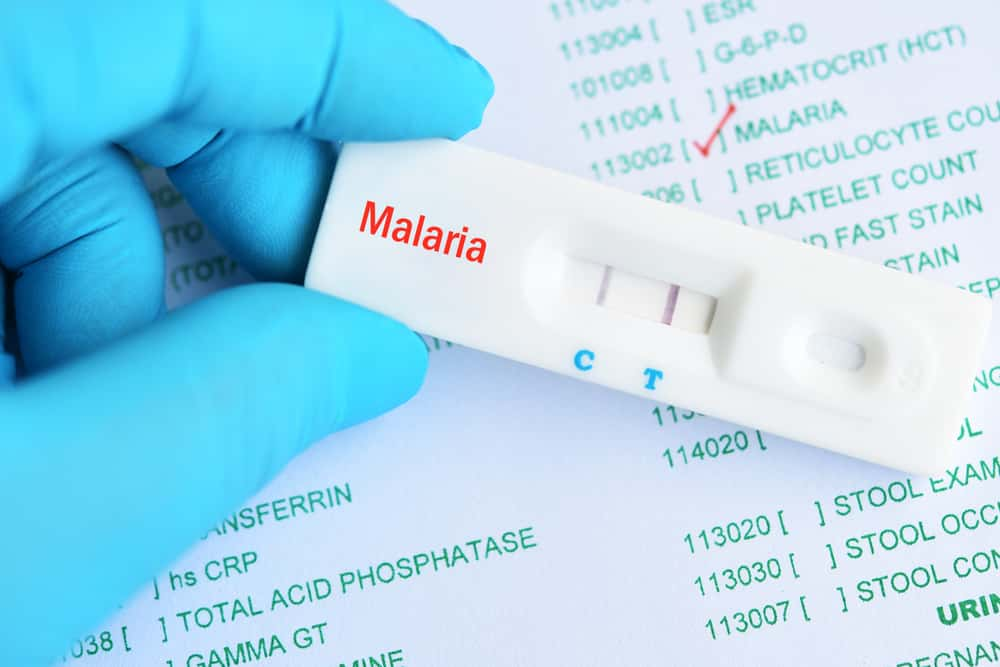
I am a doctor, but this involves my 7-year-old. 12 days ago, he started running a fever. Since we are in a malaria endemic zone, I treated for malaria and the fever subsided. Two days later he started complaining of a severe stomach ache and stooling.
I took him to the ER where I work and he was placed on some meds. For two days he seemed better, and then the pain and stooling came back with a vengeance. I took him to see a pediatrician who treated for gastritis and added another antibiotic. Both times we went to hospital he was playing and jumping around like nothing was the matter.
At 10 pm that night I couldn’t take it anymore and rushed him to the hospital, but this time to the radiology department where I pulled rank and insisted I wanted an abdominal CT scan done. And it showed an enlarged oedematous appendix.
By the next day, he was in surgery and had the appendix taken out. We are 5 days post-op now and no more pain or stooling. To put things in perspective, the CT that I insisted got done costs about $150, which where I am from is the starting monthly salary of many graduates, but I didn’t at that point think of the cost. I just knew it was something serious.
16. Off Rhythm
If you're talking in terms of diagnosis, there have been a few instances where I felt something more was going on than what others did. I worked in a 10-bed ER for many years on the night shift. When you work in a smaller hospital, you don't always have access to doctors, other than the ER doctor, and especially not to ones who practice in a certain specialty area.
The city the hospital is located in is a small college town. We often saw young college kids with one thing or another, but it was rarely serious. Over the years, I saw several college kids present with complaints of chest pain. Most of the time it was due to immense anxiety or was brought on by substances.
One night though, this 22-year-old kid came in with the same complaint. He had been in before and nothing was really off, so he was discharged with a benign prescription and was to follow up. On this visit, he was given a full cardiac workup, and nothing showed up.
Though he had chest pain before arriving, once he was in the ER it didn't occur again. Despite this, whatever he was feeling made him worry. Having no indicator of a serious issue, he was again discharged. Later in the night, around midnight, he came back in on the ambulance.
Apparently, after he left, he went home and no one had been able to reach him since. His friends or family called the authorities to do a welfare check on him and when they did, he was very out of it but quickly came around to his usual self.
By the time he got back to us, everything was again “normal". The doctor wanted to discharge him again, but my partner and I felt very strongly that something was going on with him and so we chose to keep him and observe him instead.
We placed him in a room in close proximity to the nurse’s station and left him on the telemetry monitor so that we could observe him closely. It wasn't long before he dozed off and the monitor started going off. What we saw on the monitors were these very long “pauses” until the heart would beat again.
This was a tall, fit boy with no health issues and his heart rate was in the 20s when he was asleep. We kept him all night until we could talk to his doctor in the morning. We went home and he was admitted. A few days later when we came back to work, his doctor called to tell us thank you.
She said he had been sent to a larger hospital with cardiologists and ended up getting a pacemaker put in. She said we probably saved his life. He has something called sick sinus syndrome. When he would sleep, his heart rate would drop and she said that without the welfare check he would've probably passed in his sleep.
Also, without us keeping him in the ER even after the doctor wanted to discharge him, he would've also probably passed. Nurse’s instinct, I guess.
17. Not All Discoveries Are Good
I’m an RN. I do after-hours pediatric triage nursing via telephone per diem for many years. About 5 years ago, I got a call from a parent at about 7 pm, concerned about her 5-year-old son.
He had been very tired, having frequent nosebleeds, and she called the pediatrician’s office this particular time because she also noticed a “rash” on her son. Upon further conversation with her describing the rash (flat, on the lower back, red and purple-colored) I suspected the worst. It was a sign of leukemia.
I remained calm, as mom was oblivious to the alarming symptoms her child was exhibiting, and advised her to go to the local ER immediately. My supervisor called me a few days later to inform me that the child’s pediatrician had called to commend me for my thorough and expert triage skills.
Unfortunately, the child was diagnosed with leukemia. Had I not sent him to the ER, he could have been a goner, as his platelets were dangerously low causing the nose bleeding and other symptoms.
18. It’s Worse Than It Looks
I was working in a small emergency room when we had two men brought in. They had been involved in a bar fight. One of them had been shot in the leg and the other one had been hit with a pool cue. The more senior nurse and doctor started working on the shot and I was watching the other guy.
He was talking, but for some reason he bothered me. I was getting ready to take his blood pressure when I noticed he had a slightly runny nose. I asked him if he had a cold. He didn’t, so I did what is called a “halo test” on the fluid coming out of his nose.
The test showed it was likely cerebral spinal fluid, so I immediately went and grabbed the doctor. He hadn’t actually been hit in the head with the pool cue. Instead, someone had hit him in the nose, which caused some bone to go into his brain.
We immediately flew him out to a major trauma center and it was touch and go for a long time. He did get better, which was a relief. I always wondered how it would have turned out if I hadn’t asked him a bunch of questions.
19. Looks Can Be Deceiving
A friend who did not realize I was a former surgeon was describing her issues and symptoms. Some that had been on/off for 2-3 years, but intermittent. Now they were worsening. Her family doctor (who is a friend too) suspected something innocuous.
Initially, I believe he thought it was an ulcer or pancreatitis. I knew better. Sadly, when I spoke to her, I noticed some jaundice in her eyes, and my gut feeling led me to a dark suspicion. I put in a call to my friend about my suspicion and he initially didn't agree and thought it unlikely.
She was only middle-aged, otherwise fit minus a few symptoms that had come and gone. Sadly after 2 months and with a diagnosis of pancreatic cancer she passed.
20. Nurse To Nurse
I am a nurse, and yes, I have had gut feelings, but I want to tell a story about a different nurse.
I had seen Nurse Practitioner Carol 5 months prior for my women's health exam, which was normal.
I was a busy mom—39 years old, finishing up nursing school, but had to make time for my son's ingrown toenail. While NP Carol was dealing with the toe, I happened to mention UTI symptoms that didn't get better with antibiotics.
Carol decided to examine me again. She palpated my abdomen, and “felt” something on the right side. She insisted I do an IMMEDIATE ultrasound. She was so sure, of course, I said “yes”. As soon as I saw the screen, I recognized heavy blood flow to my ovaries. My heart sank.
The total hysterectomy the following week initially came out “all clear” for cancer. I was still hospitalized when my pale-faced surgeon came to tell me early cancer cells had been found in my right ovary. It had been caught VERY early. This is quite rare.
I didn't need chemo or radiation. Carol could NOT have felt this with her fingers. She had felt it with “something else”. She had trusted her gut, and I am alive 26 years later to once again thank her for that.
21. From The Get-Go
I was doing paperwork late at night. I looked up and I saw a youngish man come in, perhaps late thirties to early forties. He walked in rather casually and did not appear distressed. But I knew that something was wrong. I grabbed a wheelchair and asked him to sit down.
Opening the door to the back, I took him to the charge nurse. I said, “This man is having a heart attack”. The nurse was used to my awareness of things and immediately put the man onto a gurney while talking to him. I returned to my desk in the front but later was told that indeed he was having a massive heart attack.
22. All’s Not Well
When I had only been a nurse for 1 and half years, I had a patient who hadn’t urinated a drop for close to 48 hours. The patient and I talked casually, and he seemed perfectly fine. However, I knew no urine meant kidney concerns.
I made a huge deal to the surgeons. I consulted the hospitalist which apparently is a ““no-no”. Only doctors can consult doctors. No one listened to me. Minimal efforts were made to justify the situation. By the end of having that patient for almost three days, he was transferred to the ICU.
I later found out he passed. Later, there was an investigation. This is what really blew my mind. The surgeons lied and said I never called them. Thankfully, my charting reflected otherwise. I was given awards for patient advocacy. However, none of that mattered to me because that patient was here one day and gone the next.
Had I been a nurse longer, I would have had the confidence to ask for more.
23. Nurses Always Know
This happened while I working in a nursing home on a weekend shift. I came in and was told a gentleman patient had a cold with fever. It was reported he was being given Tylenol and we are keeping him comfortable.
I went in to take his temperature. I found him to have been vomiting, and his temperature was 94 degrees. Now, I am a firm believer in the excellence of Tylenol, but it's not that good. It was Sunday, and calling the doctor on a Sunday doesn't usually go well. Still, I did it.
I told the doctor I couldn't say what the problem was, but this man does not have a cold. Yes, the doctor argued, “that's not possible, he has a bad cold”. I actually got to where I bet him my two weeks’ pay he doesn't have a cold. He finally let me send him out to the hospital.
Monday afternoon, my Director of Nursing called me to her office and there was the doctor who I had spent an hour convincing to send his patient out for evaluation. He had a check for me written for $1,000. His patient had a perforated viscera and the family would have sued him broke if I hadn't talked him into sending the patient out.
24. A Life-Saving Premonition
I’ll answer as a Paramedic. My gut instinct was right many times. I’ll share one story that involved 3 people with a “gut feeling” for one person. We were called to a residence at about 1 in the morning. The man who answered the door answered with an exacerbated look and said something like “I told her not to call”.
He looked ok and, with him being the only person there, we asked who called and why. About that time, his phone rang and he answered it and said “here, talk to her,” handing me the phone. I was lucky to be a double Paramedic unit and my partner continued talking to this guy while I introduced myself on the phone.
I start getting a story from the caller, who was out of state but still called 9-1-1 and got transferred to our local emergency dispatch center. She says she has known the patient for years and something is wrong with him, but she can’t specifically describe anything. Just that his voice is off, and he said a few things that were not normal.
I am listening to my partner, who’s getting nothing abnormal and his vitals are fine. I ask him if he has medications, and he directs me to the bathroom where I find blood pressure and cholesterol medications. Again, nothing is obvious on this gentleman. While he’s not saying no to us staying and checking him out, he is saying, “No I do not want to go to the hospital”.
Normally this would be clear and easy. An out-of-state call, a patient with no complaints, no obvious need for medical services…Yet something was just off. Maybe it was because he wasn’t outright saying “I don’t need you,” which most guys with no complaints would?
I asked my partner to step into the hall and she agreed she didn’t feel comfortable leaving. We sat there talking with this gentleman for over an hour (not that dispatch was happy with us), taking his vitals and keeping him on the heart monitor. At about 2 am things changed. Not often in EMS do you get to watch a patient go from normal to not normal, to full-blown crisis.
Typically we get there after the crisis. This person started by yawning a lot and trying to get his breath, and then his blood pressure shot up. He still refused to go to the hospital, and sadly he still had his mental abilities to answer questions so we couldn’t make him.
However, we got a law enforcement officer to start heading over to our location in case we needed to have a medical hold placed. Then he crashed. One second he was still talking and refusing to leave, to all of a sudden you could hear audible fluid in his lungs and he passed out.
We already knew it would happen, and like a well-oiled machine we had him on the gurney, being ventilated, IV in, and medications given. Our guy went from normal to abnormal in the back of an ambulance, and back to normal as we rolled into the doors of the ER after having gone into acute Congestive Heart Failure.
I often think of that call as I can’t ever remember any other like it. I often wonder why the patient didn’t just tell us to leave since he was so adamant on not going to the hospital. I do know he had an acute MI that night and was in the hospital for several days, but he did eventually return home.
25. It Comes At You Fast
I was working in a dialysis center, and one patient who was always jovial and a bit comedic started asking some funny questions. M. “M” was very attached to the ladies who worked there and had his favorites, but that day he asked for me instead.
He also asked if he could be a “no code” just for one day. His usual antics were still present, and he teased us that should anything happen we should just wheel him into the back room and keep on with our day.
I went to my charge nurse and expressed my concerns, but he had no symptoms that were unusual. At the end of his 4-hour treatment he sat up complaining of back pain, and slumped over...just gone. We did CPR, got him back, and lost him again.
The paramedics did the same. Long story short, he had a massive, fatal heart attack. After that happened, I learned to always follow my instincts, and keep digging for more information. Mr. M was in his early 40s, 2 weeks away from finishing college (after making a lot of bad choices early in life), and he had an appointment to see a cardiologist just 2 days later.
He knew something was wrong, and we couldn’t see it.
26. Oh, Baby
I don’t want to sound like I’m an egomaniac, but my gut feelings NEVER led me astray. When mentoring new nurses, to our unit, I emphasized this. Listen to that inner voice. I’ll give you an example. Walking into the front doors of the hospital one day, I had an impression—something bad is going to happen today.
After report, I received my assignment. My patient was attempting a VBAC (birth after cesarean). Statistics are 99 out of 100 the uterus will not rupture. Today my patient was the ONE. Her uterus, using my most accurate description, exploded during labor. The first indication was that the baby’s heart rate dropped suddenly.
Rather than wholly relying on oxygen and a wait-and-see, I stat called her MD. Physicians are required to remain on the unit during VBAC. The doctor and I whipped her into the OR. It was conveniently located around the corner and down the hall from her room.
It was fortunate that the baby by then was crowning (almost out). She was passed to the resuscitation team. Then, the MD did a manual internal check. My hand was on the patient’s abdomen as the doctor was feeling for the placenta. I nearly jumped out of my skin. I said to the doctor, “I can feel your fingers”.
Good god, the doctor’s fingers were coming out of the hole in the uterus. Only a slim thickness of the patient’s abdominal wall was between the doctor’s hand and mine. Two other nurses came into the OR to help with this possibly fatal emergency. We had two anesthesiologists by then and it was a blur of action.
I ended up donning a gown and gloves with no scrubbing of my hands. After a splash of antiseptic, the mother was opened up within a minute. The uterus looked…bad. They manually extracted the placenta. I could not believe the fabulous techniques of the obstetricians.
Somehow, they rapidly stitched up that mess into what ended up looking like a uterus. So, as you can see, yes, gut feelings happen. Looking back, I think the warning caused me to take the fast track, rather than trying to wait the problem out.
Baby heart rates regularly dip during labor. Having veteran caregivers is your best bet. They’re experts who can discern ordinary versus emergency. I was fortunate to witness new life many times in my career. Occasionally, I saw pure skill mixed with a bit of luck (or a miracle depending on your choice of words).
27. Bedside Angel
Many years ago, I was an RN in charge of a neurosurgical ward on night duty. We worked eight nights in a row, eleven-hour shifts before getting six nights off. One of our patients was being investigated for symptoms that were caused by a colloid cyst in his third ventricle.
For a couple of nights preoperatively, he had become a little agitated at two or three in the morning. So much so that I asked a junior nurse, recently returned from maternity leave, to sit by his bed on his first post-op night. My colleague and I then went to attend to patients in the acute bay who needed repositioning, chest physio, and vital signs recording.
Sitting a nurse by a patient was unusual but I had an uneasy feeling that night. As we were working, we suddenly heard a crash, glass breaking, and the nurse shouting for help. We ran to the bed to see the back and legs of the nurse, with the patient’s legs gripped in her arms as they hung over the window sill.
Glass was still hitting the pavement four floors below us. We grabbed the nurse and pulled her in. The patient stayed in her grasp and we threw him on the bed, while we made sure she was alright. She was, but the patient had broken glass in his arms and face.
That patient survived and made a complete recovery. I met him some years later at a follow-up appointment. Unusually he had complete recall of the incident but had no idea why he had done it. Had I not decided, on a whim, to sit that nurse by his bed that night, he would have perished without a doubt. A gut feeling is worth listening to.
28. Take The Wins Where You Can
You learn to trust your gut even if it means having to admit you don’t know why you feel the way you do, but you just do. I was working on the surgery floor of a busy hospital. As usual, we were short-staffed, which makes it even busier.
I had a young female patient in her early 30s who had had a bowel resection several years prior to this hospitalization. So she was actually missing several feet of her bowl. She was supposed to go down for a CT scan, but she had to drink a whole lot of contrast before she went.
It’s a little bottle of contrast in a pitcher. It’s usually Sprite or 7-Up if your nurse likes you. If you’re a jerk, it might be water. Anyway, she got the first pitcher and started gagging on the second one. She just held her tummy and looked at me and kept saying I don’t feel right.
So I went to my charge nurse and explained the situation. She called the doctor and he insisted she drink the rest of that pitcher plus one more before they would do the test. She had to have the test done before she could have surgery. She managed to get that second pitcher down, don’t know how.
By this point, I parked my med cart right outside her door and was running meds to the other patients and checking on her in between. I just had that feeling. A couple of the guys who were doing transport from downstairs came to get her. Now, when they do those tests down there on an inpatient, they send transport to get the patient ahead of time.
They then park them in the hallway in line, pretty much unattended, and that’s where they wait their turn for their test. I asked him if they had a bunch more folks lined up to go down and he said yes, but they wanted her down there and weren’t happy that she was taking so long.
I told him I would take the blame but to take the other patients first as I did not want her leaving the floor right now. I had that feeling and I didn’t want her parked in the hallway. So he left to go run other ones in. About 10 minutes after he did, she coded.
We worked on her and worked on her, and she lived long enough to make it to the ICU for her family to say their goodbyes. At least she did not pass alone in a hallway outside of a procedure room.
29. Don’t Keep Quiet
I worked as a nurse in corrections, and we had one of the patients complain of fatigue, muscle weakness, and general fatigue. He had been exercising a lot and the officers were not sure what the problem was, but he looked sick so they sent him to medical to be assessed.
We got a urine sample that was as dark as maple syrup and about as thick. We did a complete head-to-toe assessment. He had no temperature, but he looked like heck and worse by the minute. We keep telling the Officer of the day that he needed to go out, he was not stable and was tanking in front of our eyes.
He went to our Director of Nursing, who had been in corrections forever, came out and said I'm not diagnosing him, (nurses can assess but not diagnose) but I think he has Rhabdomyolyses. This is very serious and potentially fatal, so off for a ride in the ambulance he went.
They got him to the hospital and hooked him up to dialysis right away; his kidneys were failing. Come to find out, he had been feeling bad for a week and never said anything. He came very close to the end there.
30. Swinging In To Save The Day
When I had started a job working in acute medicine, we had to transfer patients up to other wards. Most of the time I would do it myself instead of waiting for a porter because it was just quicker.
While doing this once, I walked past a room of a patient I didn't know on this other ward. That’s when it hit me. I had the strangest thought: “Oh, he looks like he's bleeding somewhere”. There was no evidence though, he was just sitting and eating his lunch.
I settled my patient into their new bed and handed them over within minutes. I walked back past the room—and he was just staring at his lap while fresh blood pumped up from between his legs. I initiated the emergency call and the staff up there cracked on with hemorrhage protocol and I went back to my unit.
 Valentin Angel Fernandez , Pexels
Valentin Angel Fernandez , Pexels
31. When You Know, You Know
A woman just looked off, even though she was somehow better than she had been for 2 days. She was young, had a chest infection, and a few other bits going on, but nothing serious. She wasn't my patient, but on my unit.
I spoke to the doctor who happened to be my friend too, and I said: “I think this woman is going to go off". That's our way of saying they will have a cardiac arrest. My doctor friend just eyeballs the patient, says I'm being dramatic and she's looking good, numbers are great, no reason for worry.
Well, an hour later she’s completely hypoxic, goes blue, and arrests. No warning signs at all, I'd got the other nurse to check her really closely because of my gut feeling, and there wasn't a reason to suspect her heart would stop until she went blue and collapsed.
We did CPR and we got her to ICU and she survived. We have good reason to believe that all the rubbish she was coughing up from the infection blocked off her upper airway, causing the hypoxic arrest.
32. It Can Come From Nowhere
At my old job, we had an assessment unit for referrals from the community. This was a waiting room for about 50 people, a few bed spaces, and a triage room which was an old cubicle we converted with a desk and a trolley in it. I triaged a little old lady. She was fine, just a minor chest infection according to the doctor.
I didn't think she was right but couldn't prove it, I just felt it. This little lady needed to stay in for a day or two just to have some social problems sorted too, as well as some antibiotics. I settled her back into a big armchair and sorted her paperwork and bloodwork.
I got her a chest X-ray, and called the ward she was going to over the phone while the doctor finished writing up her examination. Well, the patient's daughter comes running out of the waiting room just then. Her news is terrifying. Apparently, her mom is blue from the waist up.
We knew then she had a pulmonary embolism. She arrests, but somehow 30 compressions and some oxygen got her back. We must have moved the clot. We got her diagnosed and treated. She was sat up, having a cup of tea half an hour after it, and we sent her over to cardiac for telemetry.
I had been watching this woman like a hawk because I just knew she wasn't ok. I wasn't the only nurse who felt it either. No reasons, we just know.
33. We’ve Got Your Back
Just the other week in my new job on intensive care, I'm looking after a post-op guy and thought “Well he looks awful,” but everything seemed ok about this man. There was no reason to think anything, and one of my colleagues said, “H's been that color since he got here".
An hour into my shift, there's blood everywhere, surgeons were up stitching his insides up on the bed where he was, and major hemorrhage protocol was activated. NEVER ignore a nurse’s gut feeling. If they say something is off, then believe it until you can disprove it.
I've been wrong with gut feelings twice maybe in 10 years and I was glad to be proven wrong! Every other time I've been spot on and it has all hit the fan, even in public spaces and at home. Because of this gut feeling, I find that my colleagues and I monitor people that bit more and we are able to act quickly.
I never ignore my nursing colleagues’ gut feelings and they don't ignore mine.
34. Inside And Out
I had a patient come in complaining of left shoulder pain. Two nights before, he had been in an auto accident and had a couple stitches and a cast on his forearm. I did vitals and his blood pressure was just a little lower than what was on his ER record.
I called his doctor, who asked me what I thought. Kind of out of nowhere, I said “a leaky spleen". He was admitted to the ICU. When the X-ray showed a huge spleen, he went to surgery and had the blood-filled spleen removed. I got a lot of praise.
35. Not Child’s Play
I worked 26 years as a psychiatric technician for the state. Multiple times during my career, I would have a gut feeling about something and go check it only to find out there was indeed something wrong.
One time, I was working on the children’s unit and my shift supervisor and I had just sat down to eat our dinner at the nursing station. I suddenly jumped up and said I want a soda….EXCEPT I don’t drink soda. I went the long way around to the soda machine, and as I walked by I was checking on “our kids".
Lo and behold, one of my boss's patients was purple-blue in color. My boss had just completed her tracheotomy care 5 minutes before, and the little girl had coughed up a mucus plug and plugged her airway. If I had dismissed my boss's protests that I didn’t drink soda, we would have lost a beautiful seven-year-old child.
36. Live And Learn
I am a government medical officer in Nepal. In Nepal, government doctors are sent to rural areas for some time before we opt for specialization. It was around 2 years ago, and I was posted in Gorkha in a remote hospital. We didn't have good labs or any scans apart from X-rays and Ultrasonography.
But we make do. We always have to. We had a female patient brought to us with loss of consciousness. At presentation she was semi-responsive, inappropriate noise to painful stimuli. Her vitals, however, were stable. Now, in rural settings, we often get females with conversion disorder (an often temporary thing) and as her vitals were normal, we thought it'd be fine by the morning.
She was brought by some friends as she was a single woman, never married, and shunned by her parents. She had left her home and had a shop that she was running on her own to earn her living. All she had were her friends, no family members.
We had a General Practitioner who was my senior there. He took a look at her and systemic examination was normal. Her labs, whatever we could do in our hospital, were normal. She responded only to painful stimuli and there was nothing to grab onto.
We admitted her, put her on IV fluids, and kept her on a catheter to monitor urine output. Her vitals were stable throughout. I examined her before the morning rounds and the thing I noticed was that her pupils were pinpoint. I immediately informed my senior.
He came and examined her yet again. She wasn't verbal and nothing in the history given by her friends was suggestive of anything. But pinpoint pupil is a concern, so we told her friends she probably needs a CT and further workup. They were reluctant to take her to a tertiary hospital. After much counseling, they were convinced and we transferred her to a tertiary center in Kathmandu. Fast forward a month later, she came to us on her own accord, healthy. And when I asked her what the doctors in the big hospital said, she said she had a small bleed in her brain. Then the whole story came out.
She apparently was depressed as her shop was not doing so well and she was in debt. Besides that, her relatives were harassing her, so she hit rock bottom. She said she had taken some pesticides, but not in a large amount. All she remembers is she took around a tablespoon full of it and she just lost consciousness.
She may have had a brain bleed due to the poison, or due to the fall, it’s hard to say. She was kept in ICU for around 4–5 days while she recovered. A psychiatric consultation was done and she was improving a little. She came to get her refill of antidepressants.
We chatted for a few minutes and she said she was feeling a bit better and her shop was doing well now. That night as I was contemplating my day as I always do, I felt like a failure because I trusted on the words of my senior and didn't examine her properly myself.
I have not met her since, as I got transferred to another hospital after that. But I still think she is one of the reasons that made me a better doctor now.
37. Working At Cross-Purposes
Some years back, I was working in an outpatient surgery center. An anesthesiologist—who I wasn’t overly fond of, nor was anyone else—brought me an older teen patient who had just had a tonsillectomy. As the patient awakened, he started coughing violently nonstop.
The anesthesiologist was standing at the foot of the gurney writing post-op medication orders for the patient and pretty much ignoring the coughing. Coughing is a really bad thing when it happens following a tonsillectomy, as it can cause the patient to begin to bleed which would require a return trip to the OR.
The surgeon came to the bedside to see the patient, as he did routinely before beginning his next case. He was obviously concerned over the violent coughing and looked at me. I knew we had codeine in our box. Codeine is the best cough suppressant when used appropriately.
I looked at the surgeon and simply said “we have codeine”. Nothing else was said as my intent was readily apparent to him, and he was a surgeon I respected. He gave me an order for how much and I went to get it.
As I walked by the anesthesiologist on the way to the box. He spoke up and said, “but I have Demerol ordered”. I just gave him “the look” and kept on going. I have no idea what was said between the two doctors. On my return, the codeine was given and the coughing stopped.
The surgeon was still there and was relieved when the coughing stopped and stayed stopped. The bottom line? The anesthesiologist was an idiot and the surgeon was appreciative of the offer that codeine was available. I am unsure if that anesthesiologist is currently practicing in the city where I encountered him.
Kudos to the surgeon who understood and accepted the offer of a medication to stop the coughing.
38. The Woman Who Cries Wolf
One of the assisted living homes that I had worked at had a resident with a history of stating, “I feel like I’m dying” or “I think I’m dying”. After lunch, she asked to lie down for a nap. Not unusual. Around 1:30 pm, she rang her call light and told me, “I think I’m dying”.
When I first walked in, for a split second it looked like she was tinged yellow. I’m not sure if that was why I believed her, or if it was her tone of voice. I remember walking out to find my co-worker walking towards her room, asking what it was that she had rang for.
I told her that she had said she thought she was dying. Then I said, “and I think she is”. The girl I was working with thought it was silly that believed her this time and brushed it off. But I knew I had to act. I grabbed the vitals supplies and walked back to her room to find her vitals perfectly normal for her baseline.
When the next shift came in at 1:45 pm, I told them the scenario and what I thought, and it was initially a repeat reaction from them as well. Still, for no physical reason, the oncoming staff/medication passer decided to send her to the hospital as a non-emergency call via ambulance.
The resident passed in the ambulance. She was a DNR but was not hospice. My administrator didn’t understand why we sent her out or why she had passed, but did tell me it saved the company because I took her vitals and we did the right thing calling the ambulance to take her to the hospital.
39. It’s Not Nothing
I am a medical office assistant, not a doctor or nurse, but I have a story to share. So, MRI is a hot commodity in my province. Incredibly long waiting lists for elective exams, sometimes over a year. I was often in charge of scheduling these.
One day a girl calls me and asks if we received her requisition. Her family doctor often drops that ball, so she was being proactive…things happen, and with wait lists this long, it doesn’t hurt to ask. Still, immediately bells go off. I don’t find it when I look.
Later that day, it comes in by fax and I grab it and send it to be approved ahead of the rest. I just had a feeling. The radiologist protocols it as elective, which means it goes into a drawer to be done as soon as we have some space, potentially a year later.
His decision makes sense. Small cyst seen on her ovary during an ultrasound 6 months previous, MRI being requested just to err on the side of caution. We would get dozens of these requests a week following pelvic ultrasounds. This had been seen during her pregnancy and was being followed-up on.
I called the patient and told her and reassured her that it was just like her general practitioner had said, it is fine. The MRI is just to be cautious and if the radiologist thought there was a risk of something severe, it never would have been prioritized as elective. This is a daily, if not hourly, conversation as an administrator in MRI.
I am not sure who I was trying to convince, her or myself. There really was no reason to be alarmed about any of it, but it just wouldn’t leave the back of my mind. A surgeon calls and cancels a patients’ MRI for the next day as the CT scan gave the doctor the information they needed.
Now, we have stacks of high-priority MRI requests to fill that slot and her exam takes a full hour. Again, I just had a feeling and felt like it should be prioritized higher. Anyone who knows anything about ovarian cancer knows that it HAS to be caught early for the patient to have a chance.
The problem is that it is usually caught too late. I take her request to the head MRI tech and she kind of looks at me like I'm crazy when I ask if I can book her. I told her that I just had a feeling and this is a 24-year-old woman with a 2-year-old and an infant. I never did this, so she allowed it. We brought her in and sure enough…it was malignant. I saved her, on a hunch.
40. Saying Goodbye
I worked in the pediatric intensive care unit as a nurse. I came in in the morning and got a report on my patient. His oxygen saturations were trending down, and the doctor made the decision to electively intubate the patient.
This means it wasn’t an emergency and we could take a few minutes to set everything up properly and not run around in emergency mode. I went out to tell his father and sister (his mother unfortunately was not there at the time). I explained that we were going to intubate him to help his breathing and we expected him to be in a medically-induced coma for a few days until his body healed enough that we could remove the breathing tube.
I asked them to come into the room and give him and hug and tell him they loved him. This was not something I normally asked parents to do prior to intubating their child. They came in and said they would see him in a couple days and then turned to leave.
I stopped them and said, “Give him a hug and tell him you love him”. They complied and left. Not 8 hours later, my teenage patient was gone. It was a horrible day, but looking back on that experience I thank God that I had the father and sister hug him one last time and tell him they loved him.
41. Going Loopy
I was taking care of a 17-year-old male who presented with psychosis. He would laugh one minute, then run down the hall. The previous shift already medicated him to help him calm down. He was not responding. Because of his erratic behavior (things like throwing himself into the wall) he was put into restraints.
He kept thrashing. I felt there was something else going on. I called the nursing supervisor and she said for me to call the on-call family medicine doctor. The doctor ordered lab work, which indicated rhabdomyolysis—a condition where damaged skeletal muscle breaks down rapidly.
The patient was transferred to a local Children’s Hospital. He was discharged several days later. He had no history of psychiatric issues, but was using steroids and working out (he was an athlete). He had drug-induced psychosis. Gut feelings are very important.
42. Everyone’s Wrong Sometimes
Unfortunately I, and many of my co-workers, all had the opposite of a gut feeling. We had a patient who was always upbeat and happy. He would come get his meds, and he was consistently doing well. He went from homeless to housed.
He was reducing his medication and stable in his life and regimen. A success story. We all adored this guy. He was friendly, kind, never made waves. He always had a nice thing to say to us nurses. He was a joy to see in a day full of often scary or difficult patients. Then it all fell apart.
It was beyond shocking when my co-worker came in and was like “Did you see the news? No? Well turn on the television”. There was our patient, caught on security cameras offing his partner.
43. Medicine As Witchcraft
I can't answer as a medic, but I can as a patient. About 28 months ago, I attended my local clinic for a scheduled post-op dressing change. A nurse I got on well with took one look at me and sent me to our hospital emergency department, phoning them herself with her suspicions.
I waited six hours to be seen. Blood was taken and when results were available, they showed my potassium level was so high I might not have survived until morning. I'm already dialysing three times weekly, but needed a lifesaving midnight 4th session to eliminate the excess.
The thing is that one of the best renal consultants in the UK and perhaps Europe knows of no way one can look at someone and see their potassium level has spiked. This wasn't nursing this was witchery! My love and gratitude to the lovely Susan!
44. The Kids Are Alright
One incident involved my father. He was in the hospital with yet another infection, which is common in kidney transplant recipients, as he was. He was close to being discharged. One night I went to visit him after work and something wasn’t right about him.
I couldn’t put my finger on it but he was “different”. The nurse caring for him that evening tried to assure me that he was okay. The next day, he was even more different, and suddenly could not transfer from the chair to the bed without a lot of help.
I told the same nurse that something was wrong and she kept insisting everything was fine—lab work, vital signs, etc. I asked her to get the doctor on the phone, and I told the doctor that “He’s not acting right, something is about to happen”.
The doctor, whom I’d worked with for many years, took my word for it and had him transferred to a more acute unit. The next day all heck literally broke loose. His transplanted kidney failed completely and he was so poisoned by toxins that he was confused.
It took several emergency dialysis sessions before he stabilized.
45. Try, Try Again
There was an elder who came in with the same complaint for quite a while. She spoke Cree only, so all conversation was done through an interpreter. The complaint was symptomatic of urinary tract infection (UTI). I did the usual urine sample testing with a culture.
The interpreter told me she said that is all we ever do for her, and the symptoms don’t get better. Red flag! So I delve into the history and explain my findings to her. She never had a urine culture come back growing anything. It isn’t a UTI.
Everyone else she saw gave her antibiotics. So now I start asking about her gynecology history, much to this lady‘s amusement. I also asked her for a pelvic exam complete with PAP smear. I fully expected to see a prolapsed uterus after finding out she was a grand multiple with 10 pregnancies or more. This would mean that the uterus was pressing on the bladder.
Only, everything looked fine on exam. I gave her medicine for the symptoms and booked her in with the doctor for a more thorough pelvic exam. Pap smear results: Carcinoma in situ. She had a doctor’s appointment and a referral for a hysterectomy.
46. A Bad Egg
I spent several years as a nurse tech, which is sort of a nurse. It was more of an orderly and unit-planning role, however. The unit was residential adolescent boys with specific intimate and social dysfunctions. I remember one patient in particular.
He came in on the morning shift, while I was off work. He had been transferred directly from a juvenile detention facility to our unit. This was contrary to appropriate practice, which was to stabilize new patients on the acute ward, then bring them in. This ward screened for erratic behavior.
The kid was huge. Seventeen years old and all of 300 pounds, every bit of it muscle. I remember talking about him in shift transfer meeting and agreeing with the other staff that this was most likely a patient who would cause trouble. Oh, if only we had known. He wouldn’t participate in treatment.
While this is common on some units, it was a rare thing in ours. Our unit had a waiting list. People in that ward usually wanted to be there. Less than a week in, we caught him carving shivs. Being the non-aggressive ward that we were, we documented it, felt unsettled and moved on.
Less than a week later, he exploded. He went after skinniest kid on the unit. I remember feeling like things went into slow motion as I saw the larger boy lunge at a boy not even half his size. They grappled, and instantly the staff went into action. I wasn’t the only one who saw it coming; another nurse, the other tech, and a therapist got on the larger boy, pulling him away.
I grabbed the skinny kid, trying to pull him free. A few frantic seconds later I had pulled him into the side hall. I asked him if he was okay. He was panting, short of breath, and sweating, but not scraped or bruised and nothing was broken. He said; “I’ve been better”.
This wasn’t my particular favorite person in treatment, but he endeared himself to me at that point. It wasn’t a fun moment to be right. It was a time I was most definitely sorry about it.
47. Full Of Hot Air
A long time ago when I was a new operating room nurse, I happened to assist a heart transplant surgery of a woman in her early 50s who had a series of surgical procedures for congenital heart anomalies. It was a very tough and risky procedure to start with, considering that there were a lot of adhesions and scarring from previous surgical operations.
The surgeon decided to place a cannula into the patient’s femoral vein for the cardio-pulmonary bypass in case he and his assistant had a hard time dissecting the veins in the chest. As they were working on the chest, trying to free up the heart, I saw something that made my stomach drop. I noticed that the patient’s belly was growing.
I cried out to the surgeon and his assistant because I suspected there was a tear in the iliac vein or somewhere. And true enough, I was right. We opened the patient’s abdomen and fixed the problem. The patient got a new heart, and the rest is history.
48. The Voice In Your Head
Sometimes you must heed that still small voice. It doesn’t shout. It won’t force your hand. Intuitively, you listen and when you learn to trust it, you must follow it. My patient Joe came to be admitted one evening accompanied by his wife, Joan.
Physically, he seemed quite well for a man of advanced age. Joe was a farmer, tall, tan, and strong with a gentle tone to his voice. He answered my questions to his ability. His wife filled in at times. His skin was warm and dry.
During his admission interview, I noticed he was fidgety. He didn’t tremble, just couldn’t be still. His wife appeared exhausted. Joe wasn’t sleeping at night and would say hurtful and shocking things about mortality. Joe interrupted himself a couple of times and mentioned to his wife how he was going to pass first.
His wife downplayed this, so I went along. Joe had been talking like this all day. Nurses know that when people talk like this who never have before, it’s something to pay attention to, no matter how unlikely it seems in reality.
Joan gave me Joe’s list of medicines. Arriving at the desk, I looked them over while notifying the doctors of his admission. His vital signs were normal, he was alert and oriented, continent, ambulatory and friendly, and verbally expressive without hesitation.
As I began to enter the medications that he took at home as protocol orders, I came across a blood thinner. Joe was taking it twice a day, and had been for a few months, for atrial fibrillation and DVT in the recent past. Joe was appropriately prescribed the medicine.
Modern “blood thinners” don’t work the same as old-fashioned ones. Blood tests usually aren’t significantly affected, and the effect usually remains for up to a week after discontinuing, to some degree.
Even so, I knew I needed to not give it to him that night. There wasn’t any measurable clinical sign of bleeding, no pallor, skin normal, dry, and Joe was gentle mannered and speaking normally, but just a bit fidgety, antsy. Most people are when they are admitted to the hospital.
They may be anxious and have a poor understanding of what’s going on, so the nurses try to put everyone at ease. No shortness of breath, no nausea or diarrhea. Pupils normal. So I told the med nurse, we’ll just start that med at 9 am, I just can’t give it tonight.
Is this a “best practice?”. I’ve been an RN for 40 years and in the field even longer. My actions may put my license on the line for anything I do or don’t do. I stand behind my decision. The next day, you can guess what happened in the early morning. Yep. Joe hemorrhaged internally.
We sent him out, after stabilizing him, to a facility better equipped to manage Joe. There really wasn’t a tremendous amount of information to support my choice. It was reasonable, though, and I knew he would still have a good pharmacological effect going on in his system without the one dose.
To me, this is a big deal, to perhaps stick my neck out. Then I think of all the educated physicians who must act on their training, knowledge of the client, and judgment in each individual choice they make for the rest of us.
The idea of their responsibility on an everyday basis is astonishing. Most of the good doctors I have known listen. They listen to that still, small voice. They make decisions that I am glad I will never have to. What would you do?
49. Listen To Your Nurses, Doctors
I was an RN on what was supposed to be the pediatric floor of a community hospital. The majority of the patients were adults, however, because I lived in an area of retired people. I was working the evening shift and a 6-month-old baby had been admitted.
His extremities were floppy, his color was gray, and he had to be in an incubator because he couldn’t maintain his body temperature. When the pediatrician came in, I told him that the baby was very ill and I had a bad feeling. I told him I thought that the infant should be transferred to the closest university hospital that had a NICU.
The doctor laughed and said the baby would be fine once he was rehydrated and the antibiotics kicked in. I told him that I had worked in NICU and I had taken care of a baby that had the same symptoms, and he was found to have infantile botulism.
The pediatrician laughed again and asked me what medical school I graduated from and reiterated that the baby would be fine with fluids and antibiotics. He left. I watched the baby like a hawk, and I could see his breathing become more labored.
I called the nursing supervisor and told her that the baby’s condition was deteriorating. She called the pediatrician and he okayed transferring the baby to the ICU. We transferred him at 9:45 pm and half an hour later, a code was called because the baby had a respiratory arrest.
The physician in the ICU called the university hospital and the baby was airlifted to a real NICU. The diagnosis: infantile botulism. The baby remained in the NICU on a ventilator for a month, but he survived and recovered without any deficits.
Shortly after that incident I moved and got a job at the university hospital.
50. So Close Yet So Far
Cardiac nurse here. A few years ago, I was taking care of a post-coronary bypass patient. He was young, active, doing great, and discharge was planned for the next day. During morning rounding, he was up in the recliner with his legs elevated, relaxing with his wife and kids.
I noticed that both his knees had large red oval-shaped pressure marks, as if he had been kneeling on the floor. I asked him if he was looking for something under the bed, and he said no. When I pointed out the red pressure marks, he said that he lays tile for a living, and that’s the exact shape of the kneepads he uses to kneel around the floor while working.
Still, he has never seen that before, and it’s been weeks since he last worked. Besides the red oval discoloration on his knees, he had no other odd signs such as mottling anywhere. He looked great, felt great, no edema or circulation issues, vitals and rhythm were great.
I communicated this odd finding to each member of his healthcare team. They each thoroughly looked him over and said to keep an eye on it overnight and to maybe keep him another day. During bedside reporting and handoff, I explained and showed this to the next nurse coming on.
In the hallway, I told her I had a funny feeling about it, and that I will be back in the morning.
During report the next morning, I found out he coded in the middle of the night and was gone. Still makes me sad to this day.
Source: 1